Abstract
Background
Laparoscopic ileostomy closure with intracorporeal anastomosis offers potential advantages over open reversal with extracorporeal anastomosis, including earlier return of bowel function and reduced postoperative pain. In this study, we aim to compare the outcome and cost of laparoscopic ileostomy reversal (utilizing either intracorporeal or extracorporeal anastomosis) with open ileostomy reversal.
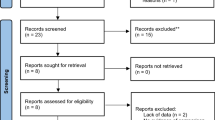
Methods
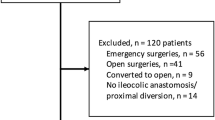
A retrospective review of sequential patients undergoing elective loop ileostomy reversal between 2013 and 2016 at a single, high-volume institution was performed. Patients were stratified on the basis of operative approach: open reversal, laparoscopic-assisted reversal with extracorporeal anastomosis (LE), and laparoscopic reversal with intracorporeal anastomosis (LI). Linear and logistic regressions were utilized to perform multivariate analysis and determine risk-adjusted outcomes.
Results
Of 132 sequential cases of loop ileostomy reversal, 50 (38%) underwent open, 49 (37%) underwent LE, and 33 (22%) underwent LI. Demographic data and preoperative comorbidities were similar between the three cohorts. Median length of stay was significantly shorter for LI (52.1 h, p < 0.05) compared to open (69.0 h) and LE (69.6 h). After risk-adjusted analysis, length of stay was significant shorter in LI compared to LE (GM 0.78, 95% CI 0.64–0.93, p < 0.01) and open reversal (GM 0.78, 95% CI 0.66–0.93, p < 0.01). Risk-adjusted 30-day morbidity rates were similar for LI compared to LE (OR 0.43, 95% CI 0.081–2.33, p = 0.33) and open reversal (OR 0.53, 95% CI 0.09–3.125, p = 0.48). Median in-hospital direct cost was similar for LI ($6575.00), LE ($6722.50), and open reversal ($6181.00).
Conclusion
Laparoscopic ileostomy reversal with intracorporeal anastomosis was associated with shorter length of stay without increased overall direct cost. The technique of laparoscopic ileostomy reversal warrants continued study in a randomized clinical trial.
Similar content being viewed by others
References
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary? Langenbeck’s Arch Surg 400:145–152
Richardson DP, Porter GA, Johnson PM (2013) Population-based use of sphincter-preserving surgery in patients with rectal cancer: is there room for improvement? Dis Colon Rectum 56:704–710
Ueno H, Mochizuki H, Hashiguchi Y et al (2004) Preoperative parameters expanding the indication of sphincter preserving surgery in patients with advanced low rectal cancer. Ann Surg 239:34–42
Park JS, Huh JW, Park YA et al (2016) Risk factors of anastomotic leakage and long-term survival after colorectal surgery. Medicine 95:e2890
Telem DA, Chin EH, Nguyen SQ, Divino CM (2010) Risk factors for anastomotic leak following colorectal surgery: a case-control study. Arch Surg (Chicago, Ill: 1960) 145:371–376 (Discussion 6)
Suding P, Jensen E, Abramson MA, Itani K, Wilson S (2008) Definitive risk factors for anastomotic leaks in elective open colorectal resection. Arch Surg 143:907–912
Midura EF, Hanseman D, Davis BR et al (2015) Risk factors and consequences of anastomotic leak after colectomy: a national analysis. Dis Colon Rectum 58:333–338
Karanjia ND, Corder AP, Bearn P, Heald RJ (1994) Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg 81:1224–1226
Wu S-W, Ma C-C, Yang Y (2014) Role of protective stoma in low anterior resection for rectal cancer: a meta-analysis. World J Gastroenterol 20:18031–18037
Choi DH, Hwang JK, Ko YT et al (2010) Risk factors for anastomotic leakage after laparoscopic rectal resection. J Korean Soc Coloproctol 26:265–273
Kim C-N (2015) Can the timing of ileostomy reversal influence functional outcome? Ann Coloproctol 31:5–6
Danielsen AK, Park J, Jansen JE et al (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265:284–290
Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF (2009) Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg 249:596–601
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Abeles A, Kwasnicki RM, Darzi A (2017) Enhanced recovery after surgery: current research insights and future direction. World J Gastrointest Surg 9:37–45
Laudicella M, Walsh B, Munasinghe A, Faiz O (2016) Impact of laparoscopic versus open surgery on hospital costs for colon cancer: a population-based retrospective cohort study. BMJ Open 6:e012977
Hellan M, Anderson C, Pigazzi A (2009) Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. J Soc Laparoendosc Surg 13:312–317
Ihnat P, Gunkova P, Peteja M, Vavra P, Pelikan A, Zonca P (2016) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30:4809–4816
Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24:711–723
Kaidar-Person O, Person B, Wexner SD (2005) Complications of construction and closure of temporary loop ileostomy. J Am Coll Surg 201:759–773
Royds J, O’Riordan JM, Mansour E, Eguare E, Neary P (2013) Randomized clinical trial of the benefit of laparoscopy with closure of loop ileostomy. Br J Surg 100:1295–1301
Russek K, George JM, Zafar N, Cuevas-Estandia P, Franklin M (2011) Laparoscopic loop ileostomy reversal: reducing morbidity while improving functional outcomes. J Soc Laparoendosc Surg 15:475–479
Young MT, Hwang GS, Menon G et al (2015) Laparoscopic versus open loop ileostomy reversal: is there an advantage to a minimally invasive approach? World J Surg 39:2805–2811
Mari GM, Crippa J, Costanzi ATM et al (2018) Intracorporeal anastomosis reduces surgical stress response in laparoscopic right hemicolectomy: a prospective randomized trial. Surg Laparosc Endosc Percutan Tech 28:77–81
Grams J, Tong W, Greenstein AJ, Salky B (2010) Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc 24:1886–1891
Crawshaw BP, Chien H, Augestad KM, Delaney CP (2015) Effect of laparoscopic surgery on health care utilization and costs in patients who undergo colectomy. JAMA Surg 150:410–415
Hiranyakas A, Rather A, da Silva G, Weiss EG, Wexner SD (2013) Loop ileostomy closure after laparoscopic versus open surgery: is there a difference? Surg Endosc 27:90–94
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Mehraneh D. Jafari receives an educational grant from Medtronic. Dr. Joseph C. Carmichael, Dr. Michael J. Stamos, Dr. Steven Mills and Dr. Alessio Pigazzi all receive an educational grant from Ethicon and Medtronic. Drs. Sarath Sujatha-Bhaskar, Matthew Whealon, Colette S. Inaba, Christina Y. Koh have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 185551 KB)
Rights and permissions
About this article
Cite this article
Sujatha-Bhaskar, S., Whealon, M., Inaba, C.S. et al. Laparoscopic loop ileostomy reversal with intracorporeal anastomosis is associated with shorter length of stay without increased direct cost. Surg Endosc 33, 644–650 (2019). https://doi.org/10.1007/s00464-018-6518-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6518-0