Abstract
Background
Non-variceal upper gastrointestinal bleeding (NVUGIB) is still a common and life-threatening disease, thus it would have a big impact on medical care cost. However, little is known about risk factors for increased medical care cost in NVUGIB patients.
Aim
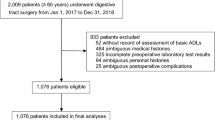
The purpose of the study was to clarify predictor of requiring high medical care cost in NVUGIB patients. Patients who underwent endoscopic hemostasis due to NVUGIB between April 2012 and March 2015 were included in this retrospective study. We analyzed the association between patients’ background including activity of daily livings (ADL) and high medical care cost using logistic regression model. Medical care cost was calculated in reference to the “Diagnosis Procedure Combination” which is diagnosis-dominant case-mix system in Japan. The cutoff value of high medical care cost was defined as its first quartile. ADL was assessed according to Katz-6 score. We defined impaired ADL patient who revealed Katz-6 score more than 1.
Results
A total of 128 consecutive patients were included in this study. Median medical care cost was 5323 USD (IQR 3661–8172 USD). There were 13 patients (10%) in impaired ADL group. In univariate analysis, age and impaired ADL before admission revealed significant association with high cost. Of these, impaired ADL was an only independent risk factor [odds ratio 15.3 (95% CI 2.49–183)] in multivariate analysis.
Conclusion
Impairment in ADL before admission was an independent predictor for high medical care cost with NVUGIB patients.

Similar content being viewed by others
References
Ministry of Health Law (2016) Estimates of national medical care expenditure, FY 2014. Ministry of Health, Labour and Welfare, Japan
Roy A, Kim M, Hawes R, Varadarajulu S (2017) The clinical and cost implications of failed endoscopic hemostasis in gastroduodenal ulcer bleeding. United Eur Gastroenterol J 5:359–364
Gagnon YM, Levy AR, Eloubeidi MA, Arguedas MR, Rioux KP, Enns RA (2003) Cost implications of administering intravenous proton pump inhibitors to all patients presenting to the emergency department with peptic ulcer bleeding. Value Health 6:457–465
Lee KK, You JH, Ho JT, Suen BY, Yung MY, Lau WH, Lee VW, Sung JY, Chan FK (2003) Economic analysis of celecoxib versus diclofenac plus omeprazole for the treatment of arthritis in patients at risk of ulcer disease. Aliment Pharmacol Ther 18:217–222
Saini SD, Schoenfeld P, Fendrick AM, Scheiman J (2008) Cost-effectiveness of proton pump inhibitor cotherapy in patients taking long-term, low-dose aspirin for secondary cardiovascular prevention. Arch Intern Med 168:1684–1690 (discussion 1691)
Edelson JT, Tosteson AN, Sax P (1990) Cost-effectiveness of misoprostol for prophylaxis against nonsteroidal anti-inflammatory drug-induced gastrointestinal tract bleeding. JAMA 264:41–47
Gan AH, Xu AG, Ling H, Chen HX, Zhang YM, Tong ZY, Zhong XH, Xu YC (2003) Value and economic analysis of emergency endoscopy in the diagnosis and treatment of massive upper gastrointestinal hemorrhage. Zhongguo wei zhong bing ji jiu yi xue = Chin Crit Care Med = Zhongguo weizhongbing jijiuyixue 15:758–761
Lee JG, Turnipseed S, Romano PS, Vigil H, Azari R, Melnikoff N, Hsu R, Kirk D, Sokolove P, Leung JW (1999) Endoscopy-based triage significantly reduces hospitalization rates and costs of treating upper GI bleeding: a randomized controlled trial. Gastrointest Endosc 50:755–761
Russo P, Brutti C (2007) Proton pump inhibitors and hospital discharge rates for gastrointestinal events in Italy: a national ecological study. Clin Ther 29:751–758
Katz S, Downs TD, Cash HR, Grotz RC (1970) Progress in development of the index of ADL. Gerontol 10:20–30
Primatesta P, Goldacre MJ, Seagroatt V (1994) Changing patterns in the epidemiology and hospital care of peptic ulcer. Int J Epidemiol 23:1206–1217
Higham J, Kang JY, Majeed A (2002) Recent trends in admissions and mortality due to peptic ulcer in England: increasing frequency of haemorrhage among older subjects. GUT 50:460–464
Kang JY, Elders A, Majeed A, Maxwell JD, Bardhan KD (2006) Recent trends in hospital admissions and mortality rates for peptic ulcer in Scotland 1982–2002. Aliment Pharmacol Ther 24:65–79
Bloom BS (1989) Risk and cost of gastrointestinal side effects associated with nonsteroidal anti-inflammatory drugs. Arch Intern Med 149:1019–1022
Motegi T, Yamada K, Kida K (2006) Cost analysis for inpatient therapy for patients with acute exacerbations of chronic obstructive pulmonary disease. Nihon Kokyuki Gakkai zasshi 44:787–794
Yagi M, Yasunaga H, Matsui H, Fushimi K, Fujimoto M, Koyama T, Fujitani J (2015) Effect of early rehabilitation on activities of daily living in patients with aspiration pneumonia. Geriatr Gerontol Int 16:1181–1187
Reed C, Belger M, Vellas B, Andrews JS, Argimon JM, Bruno G, Dodel R, Jones RW, Wimo A, Haro JM (2016) Identifying factors of activities of daily living important for cost and caregiver outcomes in Alzheimer’s disease. Int Psychogeriatr 28:247–259
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Yusaku Takatori, Motohiko Kato, Yukie Sunata, Yuichiro Hirai, Yoko Kubosawa, Keichiro Abe, Yoshiaki Takada, Tetsu Hirata, Shigeo Banno, Michiko Wada, Satoshi Kinoshita, Hideki Mori, Kaoru Takabayashi, Miho Kikuchi, Masahiro Kikuchi, Masayuki Suzuki, and Toshio Uraoka have no conflicts of interest or financial ties to disclosure.
Rights and permissions
About this article
Cite this article
Takatori, Y., Kato, M., Sunata, Y. et al. Impaired activity of daily living is a risk factor for high medical cost in patients of non-variceal upper gastrointestinal bleeding. Surg Endosc 33, 1518–1522 (2019). https://doi.org/10.1007/s00464-018-6433-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6433-4