Abstract
Background
One major adverse event of endoscopic sphincterotomy (EST) is bleeding, which could be more common and severe in patients receiving anticoagulant therapy. However, the cessation of anticoagulants for long periods could lead to thromboembolic events. We aimed to evaluate the optimal timing of resumption of anticoagulants after EST in patients at risk for thromboembolism.
Materials and methods
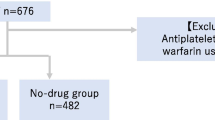
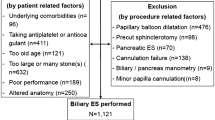
From January 2010 through October 2017, a retrospective cohort at risk for thromboembolism who had taken warfarin and bridging therapy with heparin around EST from three tertiary hospitals in South Korea was investigated. The primary outcome was to compare the incidence of post-EST delayed bleeding according to the resumption time of anticoagulant. The secondary outcome was to investigate any thromboembolic adverse events related to interruption of the anticoagulant.
Results
A total of 96 patients (46 males and 50 females; median age 75 years [range, 24–91 years]) were enrolled. Overall, the patient numbers of very early (< 24 h), early (24–48 h), and late resumption (> 48 h) of anticoagulant after EST were 56, 23, and 17, respectively. The baseline characteristics were similar between groups except resumption time of anticoagulant. There was no significant difference in the rate of post-EST delayed bleeding (5% in very early group vs. 9% in early group vs. 0 in late group, p = 0.47). The rate of thromboembolic adverse events was significantly higher in the late resumption of anticoagulant group (0 vs. 0 vs. 24%, p < 0.001).
Conclusion
There was no significant difference in the incidence of post-EST delayed bleeding according to the resuming time of anticoagulant. Since long cessation of anticoagulant could increase the risk of thrombotic adverse events, the early resumption of anticoagulant seems to be preferred.

Similar content being viewed by others
References
Acosta RD, Abraham NS, Chandrasekhara V, Chathadi KV, Early DS, Eloubeidi MA, Evans JA, Faulx AL, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Shaukat A, Shergill AK, Wang A, Cash BD, DeWitt JM (2016) The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc 83:3–16
Hamada T, Yasunaga H, Nakai Y, Isayama H, Matsui H, Horiguchi H, Fushimi K, Koike K (2015) Bleeding after endoscopic sphincterotomy or papillary balloon dilation among users of antithrombotic agents. Endoscopy 47:997–1004
Sengupta N, Feuerstein JD, Patwardhan VR, Tapper EB, Ketwaroo GA, Thaker AM, Leffler DA (2015) The risks of thromboembolism vs. recurrent gastrointestinal bleeding after interruption of systemic anticoagulation in hospitalized in patients with gastrointestinal bleeding: a prospective study. Am J Gastroenterol 110:328–335
Witt DM, Delate T, Garcia DA, Clark NP, Hylek EM, Ageno W, Dentali F, Crowther MA (2012) Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med 172:1484–1491
Staerk L, Lip GY, Olesen JB, Fosbol EL, Pallisgaard JL, Bonde AN, Gundlund A, Lindhardt TB, Hansen ML, Torp-Pedersen C, Gislason GH (2015) Stroke and recurrent haemorrhage associated with antithrombotic treatment after gastrointestinal bleeding in patients with atrial fibrillation: nationwide cohort study. BMJ 351:h5876
Veitch A, Vanbiervliet G, Gershlick A, Boustiere C, Baglin T, Smith L-A, Radaelli F, Knight E, Gralnek I, Hassan C, Dumonceau J-M (2016) Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Endoscopy 48:385–402
Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37:383–393
Lee MG, Kim J, Lee SH, Lee BS, Lee SJ, Lee YS, Cha BH, Hwang JH, Ryu JK, Kim YT (2014) Effect of sustained use of platelet aggregation inhibitors on post-endoscopic sphincterotomy bleeding. Dig Endosc 26:737–744
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R (2012) Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis., 9th edn: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e326S–e350S
Moore RA, Adel N, Riedel E, Bhutani M, Feldman DR, Tabbara NE, Soff G, Parameswaran R, Hassoun H (2011) High incidence of thromboembolic events in patients treated with cisplatin-based chemotherapy: a large retrospective analysis. J Clin Oncol 29:3466–3473
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335:909–918
Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A (1998) Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48:1–10
Hussain N, Alsulaiman R, Burtin P, Toubouti Y, Rahme E, Boivin JF, Barkun AN (2007) The safety of endoscopic sphincterotomy in patients receiving antiplatelet agents: a case-control study. Aliment Pharmacol Ther 25:579–584
Ikarashi S, Katanuma A, Kin T, Takahashi K, Yane K, Sano I, Yamazaki H, Maguchi H (2017) Factors associated with delayed hemorrhage after endoscopic sphincterotomy: Japanese large single-center experience. J Gastroenterol 52(12):1258–1265
Barthet M, Lesavre N, Desjeux A, Gasmi M, Berthezene P, Berdah S, Viviand X, Grimaud JC (2002) Complications of endoscopic sphincterotomy: results from a single tertiary referral center. Endoscopy 34:991–997
Bergman JJ, Rauws EA, Fockens P, van Berkel AM, Bossuyt PM, Tijssen JG, Tytgat GN, Huibregtse K (1997) Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet 349:1124–1129
Kim KO, Kim TN, Kim SB, Lee JY (2010) Characteristics of delayed hemorrhage after endoscopic sphincterotomy. J Gastroenterol Hepatol 25:532–538
Wilcox CM, Canakis J, Monkemuller KE, Bondora AW, Geels W (2004) Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol 99:244–248
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM, 3rd, Thomas JD (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129:e521–e643
Spyropoulos AC, Turpie AG, Dunn AS, Kaatz S, Douketis J, Jacobson A, Petersen H (2008) Perioperative bridging therapy with unfractionated heparin or low-molecular-weight heparin in patients with mechanical prosthetic heart valves on long-term oral anticoagulants (from the REGIMEN Registry). Am J Cardiol 102:883–889
Garcia DA, Regan S, Henault LE, Upadhyay A, Baker J, Othman M, Hylek EM (2008) Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med 168:63–69
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Woo Hyun Paik, Sang Hyub Lee, Dong Won Ahn, Ji Bong Jeong, Jin Woo Kang, Jun Hyuk Son, Ji Kon Ryu, and Yong-Tae Kim have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Paik, W.H., Lee, S.H., Ahn, D.W. et al. Optimal time of resuming anticoagulant after endoscopic sphincterotomy in patients at risk for thromboembolism: a retrospective cohort study. Surg Endosc 32, 3902–3908 (2018). https://doi.org/10.1007/s00464-018-6129-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6129-9