Abstract
Background
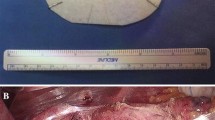
Primary repair of large hiatal hernia is associated with a high recurrence rate. The use of mesh can lead to a reduce of recurrence rate. Despite this reduction, the type of mesh used and the placement technique are controversial. In our study, we used a new type of non-absorbable, self-fixating mesh to reinforce the cruroplasty. The aim of the present study was to compare the long-term results of laparoscopic treatment of large hiatal hernia with mesh reinforcement versus simple crura repair.
Methods
This study was performed on 98 gastroesophageal reflux disease patients who underwent Nissen fundoplication with mesh-augmented crura repair and fundoplication with standard crura repair. We used non-absorbable laparoscopic self-fixating mesh by ProGrip™. All patients were separated into the mesh group (n = 50) and non-mesh group (n = 48). The groups were evaluated according to the following criteria: dysphagia, patients’ symptomatic outcome judgment according to The Gastroesophageal Reflux Disease-Health Related Quality of Life (GERD-HRQL) questionnaire and patients’ satisfaction, hiatal hernia recurrence according to upper endoscopy and a barium contrast swallow study. Follow-up was completed in 95 (97%) patients with a mean follow-up duration of 54 months (range 12–62 months).
Results
Mean operative time was not significantly different (p = 0.30302). During the 48 months of follow-up, one recurrence occurred in the mesh group and eight recurrences appeared in the non-mesh group (p = 0.027). Patient satisfaction was significantly higher in the mesh group (p = 0.004). The mesh group had a more significant improvement in GERD-HRQL score (p < 0.0001) compared to the non-mesh group.
Conclusion
In conclusion, this study confirms that laparoscopic repair of large hiatal hernias is effective and durable over a long period of time. Reinforcement of crura repair with ProGrip™ mesh is safe and can prevent anatomical recurrences.

Similar content being viewed by others
References
Kaplan JA, Schecter S, Lin MYC, Rogers SJ, Carter JT (2015) Morbidity and mortality associated with elective or emergency paraesophageal hernia repair. JAMA Surg 150:1094. https://doi.org/10.1001/jamasurg.2015.1867
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553-60-1
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439
Edelman DS (1995) Laparoscopic paraesophageal hernia repair with mesh. Surg Laparosc Endosc 5:32–37
Frantzides CT, Richards CG, Carlson MA (1999) Laparoscopic repair of large hiatal hernia with polytetrafluoroethylene. Surg Endosc 13:906–908
Paul MG, DeRosa RP, Petrucci PE, Palmer ML, Danovitch SH (1997) Laparoscopic tension-free repair of large paraesophageal hernias. Surg Endosc 11:303–307. https://doi.org/10.1007/s004649900351
Müller-Stich BP, Linke GR, Borovicka J, Marra F, Warschkow R, Lange J, Mehrabi A, Köninger J, Gutt CN, Zerz A (2008) Laparoscopic mesh-augmented hiatoplasty as a treatment of gastroesophageal reflux disease and hiatal hernias–preliminary clinical and functional results of a prospective case series. Am J Surg 195:749–756. https://doi.org/10.1016/j.amjsurg.2007.06.022
Granderath FA, Schweiger UM, Kamolz T, Pasiut M, Haas CF, Pointner R (2002) Laparoscopic antireflux surgery with routine mesh-hiatoplasty in the treatment of gastroesophageal reflux disease. J Gastrointest Surg 6:347–353
Basso N, De Leo A, Genco A, Rosato P, Rea S, Spaziani E, Primavera A (2000) 360 degrees laparoscopic fundoplication with tension-free hiatoplasty in the treatment of symptomatic gastroesophageal reflux disease. Surg Endosc 14:164–169
Granderath FA, Kamolz T, Schweiger UM, Pasiut M, Haas CF, Wykypiel H, Pointner R (2002) Long-term results of laparoscopic antireflux surgery. Surg Endosc 16:753–757. https://doi.org/10.1007/s00464-001-9103-9
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468. https://doi.org/10.1016/j.jamcollsurg.2011.05.017
Wassenaar EB, Mier F, Sinan H, Petersen RP, Martin AV, Pellegrini CA, Oelschlager BK (2012) The safety of biologic mesh for laparoscopic repair of large, complicated hiatal hernia. Surg Endosc 26:1390–1396. https://doi.org/10.1007/s00464-011-2045-y
Oelschlager BK, Barreca M, Chang L, Pellegrini CA (2003) The use of small intestine submucosa in the repair of paraesophageal hernias: initial observations of a new technique. Am J Surg 186:4–8
Frantzides CT, Carlson MA, Loizides S, Papafili A, Luu M, Roberts J, Zeni T, Frantzides A (2010) Hiatal hernia repair with mesh: a survey of SAGES members. Surg Endosc 24:1017–1024. https://doi.org/10.1007/s00464-009-0718-6
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548. https://doi.org/10.1007/s00464-006-9041-7
Bonrath EM, Grantcharov TP (2015) Contemporary management of paraesophaegeal hernias: establishing a European expert consensus. Surg Endosc 29:2180–2195. https://doi.org/10.1007/s00464-014-3918-7
Huddy JR, Markar SR, Ni MZ, Morino M, Targarona EM, Zaninotto G, Hanna GB (2016) Laparoscopic repair of hiatus hernia: Does mesh type influence outcome? A meta-analysis and European survey study. Surg Endosc 30:5209–5221. https://doi.org/10.1007/s00464-016-4900-3
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R, Frantzides CT (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20:367–379. https://doi.org/10.1007/s00464-005-0467-0
Tatum RP, Shalhub S, Oelschlager BK, Pellegrini CA (2008) Complications of PTFE mesh at the diaphragmatic hiatus. J Gastrointest Surg 12:953–957. https://doi.org/10.1007/s11605-007-0316-7
Lee E, Frisella MM, Matthews BD, Brunt LM (2007) Evaluation of acellular human dermis reinforcement of the crural closure in patients with difficult hiatal hernias. Surg Endosc 21:641–645. https://doi.org/10.1007/s00464-006-9117-4
Zilberstein B, Eshkenazy R, Pajecki D, Granja C, Brito ACG (2005) Laparoscopic mesh repair antireflux surgery for treatment of large hiatal hernia. Dis Esophagus 18:166–169. https://doi.org/10.1111/j.1442-2050.2005.00494.x
Willekes CL, Edoga JK, Frezza EE (1997) Laparoscopic repair of paraesophageal hernia. Ann Surg 225:31–38
Zhang W, Tang W, Shan C-X, Liu S, Jiang Z-G, Jiang D-Z, Zheng X-M, Qiu M (2013) Dual-sided composite mesh repair of hiatal hernia: our experience and a review of the Chinese literature. World J Gastroenterol 19:5528. https://doi.org/10.3748/wjg.v19.i33.5528
Kohn GP, Price RR, DeMeester SR, Zehetner J, Muensterer OJ, Awad Z, Mittal SK, Richardson WS, Stefanidis D, Fanelli RD, SAGES Guidelines Committee (2013) Guidelines for the management of hiatal hernia. Surg Endosc 27:4409–4428. https://doi.org/10.1007/s00464-013-3173-3
Wang B, Zhang W, Shan C, Liu S, Jiang Z, Qiu M (2016) Long-term outcomes of cruroplasty reinforcement with composite versus biologic mesh for gastroesophageal reflux disease. Surg Endosc 30:2865–2872. https://doi.org/10.1007/s00464-015-4570-6
Granderath FA (2007) Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why when how? Surg Endosc 21:2224–2225. https://doi.org/10.1007/s00464-007-9348-z
Grubnik VV, Malynovskyy AV (2013) Laparoscopic repair of hiatal hernias: new classification supported by long-term results. Surg Endosc 27:4337–4346. https://doi.org/10.1007/s00464-013-3069-2
Granderath F, Kamolz T, Schweiger UM, Pointner R (2003) Laparoscopic refundoplication with prosthetic hiatal closure for recurrent hiatal hernia after primary failed antireflux surgery. Arch Surg 138:902. https://doi.org/10.1001/archsurg.138.8.902
Carlson MA, Condon RE, Ludwig KA, Schulte WJ (1998) Management of intrathoracic stomach with polypropylene mesh prosthesis reinforced transabdominal hiatus hernia repair. J Am Coll Surg 187:227–230
Ward KC, Costello KP, Baalman S, Pierce RA, Deeken CR, Frisella MM, Michael Brunt L, Matthews BD (2015) Effect of acellular human dermis buttress on laparoscopic hiatal hernia repair. Surg Endosc 29:2291–2297. https://doi.org/10.1007/s00464-014-3946-3
Gonzalez R, Fugate K, McClusky D, Ritter EM, Lederman A, Dillehay D, Smith CD, Ramshaw BJ (2005) Relationship between tissue ingrowth and mesh contraction. World J Surg 29:1038–1043. https://doi.org/10.1007/s00268-005-7786-0
Furnée E, Hazebroek E (2013) Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc 27:3998–4008. https://doi.org/10.1007/s00464-013-3036-y
Korolija D, Sauerland S, Wood-Dauphine S, Abbou CC, Eypasch E, Caballero MG, Lumsden MA, Millat B, Monson JRT, Nilsson G, Pointner R, Schwenk W, Shamiyeh A, Szold A, Targarona E, Ure B, Neugebauer E, European Association for Endoscopic Surgery (2004) Evaluation of quality of life after laparoscopic surgery: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc 18:879–897. https://doi.org/10.1007/s00464-003-9263-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
V. V. Ilyashenko, Viktor V. Grubnyk, and V. V. Grubnik have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ilyashenko, V.V., Grubnyk, V.V. & Grubnik, V.V. Laparoscopic management of large hiatal hernia: mesh method with the use of ProGrip mesh versus standard crural repair. Surg Endosc 32, 3592–3598 (2018). https://doi.org/10.1007/s00464-018-6087-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6087-2