Abstract
Background
Few data are available concerning short-term results of minimally invasive surgery in patients > 70 years old requiring distal pancreatectomy. The aim of this study was to compare short-term results after laparoscopic (LDP) versus open distal pancreatectomy (ODP) in this subgroup of patients.
Methods
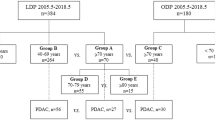
All patients > 70 years who underwent distal pancreatectomy in 3 expert centers between 1995 and 2017 were included and data were retrospectively analyzed. Demographic, intraoperative data and postoperative outcomes in LDP and ODP groups were compared.
Results
A distal pancreatectomy was performed in 109 elderly patients; LDP group included 53 patients while ODP group included 56. There were 55 (50.5%) males and 54 (49.5%) women with a median age of 75 years (range 70–87). Fifty (45.9%) patients were 70–74, 40 (36.7%) patients were 75–79, and 19 (17.4%) patients were over 80 years. Nine (8.2%) patients required conversion to open surgery. The median operative time was not different between LDP and ODP (204 vs. 220 min, p = 0.62). The intraoperative blood loss was significantly lower in the LDP group (238 ± 312 vs. 425 ± 582 ml, p = 0.009) with no difference regarding the intraoperative transfusion rate. 90-day mortality (0 vs. 5%, p = 0.42), overall complication (45.4 vs. 51.8%, p = 0.53), major complication (18.2 vs. 12.5%, p = 0.43), grade B/C pancreatic fistula (6.8 vs. 7.1%, p = 0.71), were comparable in the 2 groups. Only postoperative confusion rate was significantly lower in the LDP group (4.5 vs. 25%, p = 0.01). Median length of stay was significantly lower in the LDP group (14 ± 10 vs. 16 ± 11 days, p = 0.04). R0 resection was performed in 94% of LDP patients and 89% in ODP patients without significant difference (p = 0.73).
Conclusions
The laparoscopic approach seems to reduce blood loss, postoperative confusion, and length of stay in elderly patients requiring distal pancreatectomy.


Similar content being viewed by others
References
Riviere D, Gurusamy KS, Kooby DA, Vollmer CM, Besselink MG, Davidson BR et al (2016) Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev 4:CD011391
Edwin B, Sahakyan MA, Hilal MA, Besselink MG, Braga M, Fabre JM et al.Laparoscopic surgery for pancreatic neoplasms: the European association for endoscopic surgery clinical consensus conference. Surg Endosc. 2017
Shin SH, Kim SC, Song KB, Hwang DW, Lee JH, Park KM et al (2016) Appraisal of laparoscopic distal pancreatectomy for left-sided pancreatic cancer: a large volume cohort study of 152 consecutive patients. PLoS ONE 11(9):e0163266
Nakamura M, Nakashima H (2013) Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci 20(4):421–428
Nakamura M, Wakabayashi G, Miyasaka Y, Tanaka M, Morikawa T, Unno M et al (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepatobiliary Pancreat Sci 22(10):731–736
Mehta SS, Doumane G, Mura T, Nocca D, Fabre JM (2012) Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surg Endosc 26(2):402–407
Liang S, Hameed U, Jayaraman S (2014) Laparoscopic pancreatectomy: indications and outcomes. World J Gastroenterol 20(39):14246–14254
Fong Y, Blumgart LH, Fortner JG, Brennan MF (1995) Pancreatic or liver resection for malignancy is safe and effective for the elderly. Ann Surg 222(4):426–434. (discussion 34–37)
Yeo CJ, Sohn TA, Cameron JL, Hruban RH, Lillemoe KD, Pitt HA (1998) Periampullary adenocarcinoma: analysis of 5-year survivors. Ann Surg 227(6):821–831
Balcom JHT, Rattner DW, Warshaw AL, Chang Y, Fernandez-del Castillo C (2001) Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg 136(4):391–398
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J et al (2006) 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10(9):1199–1210. (discussion 210–211)
Makary MA, Winter JM, Cameron JL, Campbell KA, Chang D, Cunningham SC et al (2006) Pancreaticoduodenectomy in the very elderly. J Gastrointest Surg 10(3):347–356
Sohn TA, Yeo CJ, Cameron JL, Lillemoe KD, Talamini MA, Hruban RH et al (1998) Should pancreaticoduodenectomy be performed in octogenarians? J Gastrointest Surg 2(3):207–216
Scurtu R, Bachellier P, Oussoultzoglou E, Rosso E, Maroni R, Jaeck D (2006) Outcome after pancreaticoduodenectomy for cancer in elderly patients. J Gastrointest Surg 10(6):813–822
Riall TS, Reddy DM, Nealon WH, Goodwin JS (2008) The effect of age on short-term outcomes after pancreatic resection: a population-based study. Ann Surg 248(3):459–467
Bathe OF, Levi D, Caldera H, Franceschi D, Raez L, Patel A et al (2000) Radical resection of periampullary tumors in the elderly: evaluation of long-term results. World J Surg 24(3):353–358
Brozzetti S, Mazzoni G, Miccini M, Puma F, De Angelis M, Cassini D et al (2006) Surgical treatment of pancreatic head carcinoma in elderly patients. Arch Surg 141(2):137–142
Sukharamwala P, Thoens J, Szuchmacher M, Smith J, DeVito P (2012) Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB 14(10):649–657
Casadei R, Ricci C, Lazzarini E, Taffurelli G, D’Ambra M, Mastroroberto M et al (2014) Pancreatic resection in patients 80 years or older: a meta-analysis and systematic review. Pancreas 43(8):1208–1218
Kawaguchi Y, Fuks D, Nomi T, Levard H, Gayet B (2015) Laparoscopic distal pancreatectomy employing radical en bloc procedure for adenocarcinoma: technical details and outcomes. Surgery 157(6):1106–1112
Sanchez-Cabus S, Adam JP, Pittau G, Gelli M, Cunha AS (2016). Laparoscopic left pancreatectomy: early results after 115 consecutive patients. Surg Endosc 30(10):4480–4488
Kimura W, Yano M, Sugawara S, Okazaki S, Sato T, Moriya T et al (2010) Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance. J Hepatobiliary Pancreat Sci 17(6):813–823
Warshaw AL (1988) Conservation of the spleen with distal pancreatectomy. Arch Surg 123(5):550–553
Strasberg SM, Linehan DC, Hawkins WG (2007) Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg 204(2):244–249
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Brouquet A, Cudennec T, Benoist S, Moulias S, Beauchet A, Penna C et al (2010) Impaired mobility, ASA status and administration of tramadol are risk factors for postoperative delirium in patients aged 75 years or more after major abdominal surgery. Ann Surg 251(4):759–765
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Mise Y, Day RW, Vauthey JN, Brudvik KW, Schwarz L, Prakash L et al. (2015) After pancreatectomy, the “90 days from surgery” definition is superior to the “30 days from discharge” definition for capture of clinically relevant readmissions. J Gastrointest Surg 20(1):77–84
Jusoh AC, Ammori BJ (2012) Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. Surg Endosc 26(4):904–913
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255(6):1048–1059
Sui CJ, Li B, Yang JM, Wang SJ, Zhou YM (2012) Laparoscopic versus open distal pancreatectomy: a meta-analysis. Asian J Surg 35(1):1–8
Sahakyan MA, Edwin B, Kazaryan AM, Barkhatov L, Buanes T, Ignjatovic D et al (2017) Perioperative outcomes and survival in elderly patients undergoing laparoscopic distal pancreatectomy. J Hepatobiliary Pancreat Sci 24(1):42–48
Yi X, Chen S, Wang W, Zou L, Diao D, Zheng Y et al. (2017) A systematic review and meta-analysis of laparoscopic and open distal pancreatectomy of nonductal adenocarcinomatous pancreatic tumor (NDACPT) in the pancreatic body and tail. Surg Laparosc Endosc Percutan Tech 27(4):206–219
Kim SC, Park KT, Hwang JW, Shin HC, Lee SS, Seo DW et al (2008) Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 22(10):2261–2268
Teh SH, Tseng D, Sheppard BC (2007) Laparoscopic and open distal pancreatic resection for benign pancreatic disease. J Gastrointest Surg 11(9):1120–1125
Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC (2002) The value of splenic preservation with distal pancreatectomy. Arch Surg 137(2):164–168
Kleeff J, Diener MK, Z’Graggen K, Hinz U, Wagner M, Bachmann J et al (2007) Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 245(4):573–582
Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH et al (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143(10):956–965
Kneuertz PJ, Patel SH, Chu CK, Fisher SB, Maithel SK, Sarmiento JM et al (2012) Laparoscopic distal pancreatectomy: trends and lessons learned through an 11-year experience. J Am Coll Surg 215(2):167–176
Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Schmidt MC, Merchant NB et al (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248(3):438–446
Finlayson E, Fan Z, Birkmeyer JD (2007) Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg 205(6):729–734
Khan S, Sclabas G, Lombardo KR, Sarr MG, Nagorney D, Kendrick ML et al (2010) Pancreatoduodenectomy for ductal adenocarcinoma in the very elderly; is it safe and justified? J Gastrointest Surg 14(11):1826–1831
Magge D, Gooding W, Choudry H, Steve J, Steel J, Zureikat A et al (2013) Comparative effectiveness of minimally invasive and open distal pancreatectomy for ductal adenocarcinoma. JAMA Surg 148(6):525–531
Duran H, Ielpo B, Caruso R, Ferri V, Quijano Y, Diaz E et al (2014) Does robotic distal pancreatectomy surgery offer similar results as laparoscopic and open approach? A comparative study from a single medical center. Int J Med Robot 10(3):280–285
Marangos IP, Buanes T, Rosok BI, Kazaryan AM, Rosseland AR, Grzyb K et al (2012) Laparoscopic resection of exocrine carcinoma in central and distal pancreas results in a high rate of radical resections and long postoperative survival. Surgery 151(5):717–723
Kang CM, Lee SH, Lee WJ (2014) Minimally invasive radical pancreatectomy for left-sided pancreatic cancer: current status and future perspectives. World J Gastroenterol 20(9):2343–2351
Kang CM, Kim DH, Lee WJ (2010) Ten years of experience with resection of left-sided pancreatic ductal adenocarcinoma: evolution and initial experience to a laparoscopic approach. Surg Endosc 24(7):1533–1541
Song KB, Kim SC, Park JB, Kim YH, Jung YS, Kim MH et al (2011) Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc 25(10):3364–3372
Hu M, Zhao G, Wang F, Zhao Z, Li C, Liu R (2014) Laparoscopic versus open distal splenopancreatectomy for the treatment of pancreatic body and tail cancer: a retrospective, mid-term follow-up study at a single academic tertiary care institution. Surg Endosc 28(9):2584–2591
Sahakyan MA, Kim SC, Kleive D, Kazaryan AM, Song KB, Ignjatovic D et al. (2017) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: long-term oncologic outcomes after standard resection. Surgery 162(4):802–811
Sulpice L, Farges O, Goutte N, Bendersky N, Dokmak S, Sauvanet A et al. (2015) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: time for a randomized controlled trial? results of an all-inclusive national observational study. Ann Surg 262(5):868–873. (discussion 73–74)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs Souche, Fuks, Perinel, Herrero, Guillon, Pirlet, Perniceni, Borie, Sa Cunha, Gayet, and Fabre have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Souche, R., Fuks, D., Perinel, J. et al. Impact of laparoscopy in patients aged over 70 years requiring distal pancreatectomy: a French multicentric comparative study. Surg Endosc 32, 3164–3173 (2018). https://doi.org/10.1007/s00464-018-6033-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6033-3