Abstract
Background
Single-incision distal gastrectomy (SIDG) is technically difficult due to limited range of motion and unstable field of view. Solo surgery using a passive scope holder may be the key in allowing SIDG to be safer and efficient. We report our initial 100 cases of, to what we know, the world’s first solo SIDG, and calculate the learning curve.
Methods
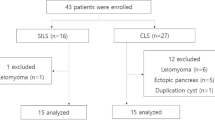
Prospectively collected database of 100 patients clinically diagnosed as gastric cancer who underwent solo SIDG from October 2013 until July 2016 was analyzed. All the operations were held by a single surgeon with no assistants. A passive laparoscopic scope holder was used to fix the field of view.
Results
The mean operation time was 120.6 ± 30.2 min, and the average estimated blood loss was 33.5 ± 55.7 ml. Average body mass index was 23.4 ± 2.9 kg/m2. The median hospital stay was 5 (4–14) days, and the mean number of retrieved lymph nodes was 56.0 ± 22.8. There was no conversion to multiport or open surgery. Early complication of Clavien–Dindo grade III or more was 3%. Learning curve was calculated on operation time, and showed that an experienced surgeon in SIDG required 20 cases or less in stabilizing the operation time for solo SIDG.
Conclusions
Solo SIDG seems to be feasible and safe. The stable field of view created by a scope holder provides a favorable environment for a finer and more consistent operation. In addition, manpower can also be saved without affecting the quality of surgery.




Similar content being viewed by others
References
Tacchino R, Greco F, Matera D (2009) Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc 23:896–899
Kim S-J, Choi B-J, Lee SC (2015) Novel approach of single-port laparoscopic appendectomy as a solo surgery: a prospective cohort study. Int J Surg 21:1–7
Law WL, Fan JKM, Poon JTC (2009) Single incision laparoscopic left colectomy for carcinoma of distal transverse colon. Colorectal Dis 12:698–701
Park YS, Park DJ, Kim KH, Park DJ, Ahn S-H, Kim H-H (2015) Single incisional laparoscopic sleeve gastrectomy and adolescent bariatric surgery: case report and brief review. J Metab Bariatr Surg 4:40–45
Romanelli JR, Earle DB (2009) Single-port laparoscopic surgery: an overview. Surg Endosc 23:1419–1427
Lakdawala M, Agarwal A, Dhar S, Dhulla N, Remedios C, Bhasker AG (2015) Single-incision sleeve gastrectomy versus laparoscopic sleeve gastrectomy. A 2-year comparative analysis of 600 patients. Obes Surg 25:607–614
Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T (2011) Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc 25:2400–2404
Ahn S-H, Park DJ, Son S-Y, Lee C-M, Kim H-H (2013) Single-incision laparoscopic total gastrectomy with D1 + beta lymph node dissection for proximal early gastric cancer. Gastric Cancer 17:392–396
Park DJ, Lee J-H, Ahn S-H, Eng AKH, Kim H-H (2012) Single-port laparoscopic distal gastrectomy with D1 + β lymph node dissection for gastric cancers. Surg Laparosc Endosc Percutan Tech 22:e214–e216
Ahn S-H, Son S-Y, Jung DH, Park DJ, Kim H-H (2014) Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg 219:933–943
Choi B-J, Jeong WJ, Kim S-J, Lee SC (2017) Solo-surgeon single-port laparoscopic anterior resection for sigmoid colon cancer: comparative study. J Laparoendosc Adv Surg Tech 28:330–336
Fujii S, Watanabe K, Ota M, Yamagishi S, Kunisaki C, Osada S, Ike H, Ichikawa Y, Endo I, Shimada H (2011) Solo surgery in laparoscopic colectomy: a case-matched study comparing robotic and human scopist. Hepatogastroenterology 58:406–410
Kang SH, Lee Y, Park YS, Ahn S-H, Park DJ, Kim H-H (2017) Solo single-incision laparoscopic resectional Roux-en-Y gastric bypass for morbid obesity with metabolic syndrome. Obes Surg 27:3314–3319
Shabbir A, Lee J-H, Lee M-S, Park DJ, Kim H-H (2010) Combined suture retraction of the falciform ligament and the left lobe of the liver during laparoscopic total gastrectomy. Surg Endosc 24:3237–3240
Kodera Y, Sano T (2016) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–19
Irino T (2015) The Hit and Away technique: optimal usage of the ultrasonic scalpel in laparoscopic gastrectomy. Surg Endosc 30:1–6
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo Classification of surgical complications. Ann Surg 250:187–196
Poon JTC, Cheung C-W, Fan JKM, Lo OSH, Law W-L (2012) Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 26:2729–2734
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24:1842–1848
Chambers WM, Bicsak M, Lamparelli M, Dixon AR (2011) Single-incision laparoscopic surgery (SILS) in complex colorectal surgery: a technique offering potential and not just cosmesis. Colorectal Dis 13:393–398
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2012) Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 26:1205–1213
Abdelrahman AM, Bingener J, Yu D, Lowndes BR, Mohamed A, McConico AL, Hallbeck MS (2016) Impact of single-incision laparoscopic cholecystectomy (SILC) versus conventional laparoscopic cholecystectomy (CLC) procedures on surgeon stress and workload: a randomized controlled trial. Surg Endosc 30:1205–1211
Yang YS, Kim SH, Jin CH, Oh KY, Hur MH, Kim SY, Yim HS (2014) Solo surgeon single-port laparoscopic surgery with a homemade laparoscope-anchored instrument system in benign gynecologic diseases. J Minim Invasive Gynecol 21:695–701
Kim W, Kim H-H, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang H-K, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee H-J, Korean Laparo-endoscopic Gastrointestinal Surgery Study (KLASS) Group (2016) decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a Multicenter Randomized Controlled Trial (KLASS-01). Ann Surg 263:28–35
Lee B, Lee YT, Park YS, Ahn S-H, Park DJ, Kim H-H (2018) Learning curve of pure single-port laparoscopic distal gastrectomy for gastric cancer. J Gastric Cancer 18:182–188
Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE, Bonham Group (2016) Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20:1–10
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
So Hyun Kang, Yo-Seok Cho, Sa-Hong Min, Young Suk Park, Sang-Hoon Ahn, Do Joong Park, and Hyung-Ho Kim have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, S.H., Cho, YS., Min, SH. et al. Early experience and learning curve of solo single-incision distal gastrectomy for gastric cancer: a review of consecutive 100 cases. Surg Endosc 33, 3412–3418 (2019). https://doi.org/10.1007/s00464-018-06638-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06638-1