Abstract
Background
Morbidly obese patients are at increased risk for venous thromboembolism (VTE) after bariatric surgery. Perioperative chemoprophylaxis is used routinely with bariatric surgery to decrease the risk of VTE. When bleeding occurs, routine chemoprophylaxis is often withheld due to concerns about inciting another bleeding event. We sought to evaluate the relationship between perioperative bleeding and postoperative VTE in bariatric surgery.
Methods
The American College of Surgeons-National Surgical Quality Improvement Program (NSQIP) dataset between 2012 and 2014 was queried to identify patients who underwent bariatric surgery. Gastric bypass (n = 28,145), sleeve gastrectomy (n = 30,080), bariatric revision (n = 324), and biliopancreatic diversion procedures (n = 492) were included. Univariate and multivariate regressions were used to determine perioperative factors predictive of postoperative VTE within 30 days in patients who experience a bleeding complication necessitating transfusion.
Results
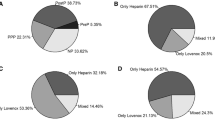
The rate of bleeding necessitating transfusion was 1.3%. Bleeding was significantly more likely to occur in gastric bypass compared to sleeve gastrectomy (1.6 vs. 1.0%) (p < 0.0001). For all surgeries, increased age, length of stay, operative time, and comorbidities including hypertension, dyspnea with moderate exertion, partially dependent functional status, bleeding disorder, transfusion prior to surgery, ASA class III/IV, and metabolic syndrome increased the perioperative bleeding risk (p < 0.05). Multivariate analysis revealed that the rate of VTE was significantly higher after blood transfusion [Odds Ratio (OR) = 4.7; 95% CI 2.9–7.9; p < 0.0001). Predictive risk factors for VTE after transfusion included previous bleeding disorder, ASA class III or IV, and COPD (p < 0.05).
Conclusions
Bariatric surgery patients who receive postoperative blood transfusion are at a significantly increased risk for VTE. The etiology of VTE in those who are transfused is likely multifactorial and possibly related to withholding chemoprophylaxis and the potential of a hypercoagulable state induced by the transfusion. In those who bleed, consideration should be given to reinitiating chemoprophylaxis when safe, extending treatment after discharge, and screening ultrasound.


Similar content being viewed by others
References
Buchwald H, Oien DM (2009) Metabolic/bariatric surgery worldwide. Obes Surg 19(12):1605–1611
American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2013) American society of metabolic and bariatric surgery position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis 9(4):493–497
Morino M, Topinno M, Forestieri P, Angrisani L, Allaix ME, Scopinaro N (2007) Mortality after bariatric surgery: analysis of 13,871 morbidly obese patients from a National Registry. Ann Surg 246(6):1002–1007
https://asmbs.org/resources/cpt-and-icd-9-codes-for-bariatric-surgery. Accessed 27 Sept 2017
Aminian A, Andalib A, Khorgami Z, Cetin D, Burguera B, Bartholomew J, Brethauer SA, Schauer PR (2017) Who should get extended thromboprophylaxis after bariatric surgery? A risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg 265:143–150
Mandala M, Falanga A, Roila F (2011) Management of venous thromboembolism (VTE) in cancer patients: ESMO Clinical Practice Guidelines. Ann Onc 22(6):85–92
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ (2010) The metabolic syndrome. Lancet 375(9710):181–183
Zellmer JD, Mathiason MA, Kallies KJ, Kothari SN (2014) Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg 208(6):903–910
Janik MR, Walędziak M, Brągoszewski J, Kwiatkowski A, Paśnik K (2017) Prediction model for hemorrhagic complications after laparoscopic sleeve gastrectomy: development of SLEEVE BLEED calculator. Obes Surg 27(4):968–972
Stamou KM, Menenakos E, Dardamanis D, Arabatzi C, Alevizos L, Albanopoulos K, Leandros E, Zografos G (2011) Prospective comparative study of the efficacy of staple-line reinforcement in laparoscopic sleeve gastrectomy. Surg Endosc 25(11):3526–3530
Ichter ZA, Voeller L, Rivas H, Khoury H, Azagury D, Morton JM (2017) Buttressing of the EEA stapler during gastrojejunal anastomosis decreases rate of bleeding-related complications for laparoscopic gastric bypass. Surg Obes Relat Dis 13(5):802–806
Berger ER, Huffman KM, Fraker T, Petrick AT, Brethauer SA, Hall BL, Ko CY, Morton JM (2016) Prevalence and risk factors for bariatric surgery readmissions: findings from 130,007 admissions in the metabolic and bariatric surgery accreditation and quality improvement program. Ann Surg. https://doi.org/10.1097/SLA.0000000000002079
Thereaux J, Lesuffleur T, Czernichow S, Basdevant A, Msika S, Nocca D, Millat B, Fagot-Campagna A (2017) To what extent does post-hospital discharge chemoprophylaxis prevent venous thromboembolism after bariatric surgery? Results from a nationwide cohort of more than 110,000 patients. Ann Surg. https://doi.org/10.1097/SLA.0000000000002285
Rowland SP, Dharmarajah B, Moore HM, Lane TR, Cousins J, Ahmed AR, Davies AH (2015) Inferior vena cava filters for prevention of venous thromboembolism in obese patients undergoing bariatric surgery: a systematic review. Ann Surg 261(1):35–45
Khorana AA, Francis CW, Blumberg N, Culakova E, Refaai MA, Lyman GH (2008) Blood transfusions, thrombosis, and mortality in hospitalized patients with cancer. Arch Intern Med 168(21):2377–2381
Xenos ES, Vargas HD, Davenport DL (2012) Association of blood transfusion and venous thromboembolism after colorectal cancer resection. Thromb Res 129(5):568–572
Abu-Rustum NR, Richard S, Wilton A, Lev G, Sonoda Y, Hensley ML, Genignani M, Barakat RR, Chi DS (2005) Transfusion utilization during adnexal or peritoneal cancer surgery: effects on symptomatic venous thromboembolism and survival. Gynecol Oncol 99(2):320–326
Sillman CC, Moore EE, Johnson JL, Gonzalez RJ, Biffl WL (2004) Transfusion of the injured patient: proceed with caution. Shock 21(4):291–299
Knudson MM, Collins JA, Goodman SB, McCrory DW (1992) Thromboembolism following multiple trauma. J Trauma 32(1):2–11
Zallen G, Moore EE, Ciesla DJ, Brown M, Biffl WL, Sillman CC (2000) Stored red blood cells selectively activate human neutrophils to release IL-8 and secretory PLA2. Shock 13(1):29–33
Park MS, Martini WZ, Dubick MA, Salinas J, Butenas S, Kheirabadi BS, Pusateri AE, Vos JA, Guymon CH, Wolf SE, Mann KG, Holcomb JB (2009) Thromboelastography as a better indicator of hypercoagulable state after injury than prothrombin time or activated partial thromboplastin time. J Trauma 67(2):266–76
Finks JF, English WJ, Carlin AM, Krause KR, Share DA, Banerjee M, Birkmeyer JD, Birkmeyer NJ, Michigan Bariatric Surgery Collaborative; Center for Healthcare Outcomes and Policy (2012) Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan bariatric surgery collaborative. Ann Surg 255(6):1100–1104
Freeman AL, Pendleton RC, Rondina MT (2010) Prevention of venous thromboembolism in obesity. Expert Rev Cardiovasc Ther 8(12):1711–1721
Lopez JA, Chen J (2009) Pathophysiology of venous thrombosis. Thromb Res 123:S30–S34
Funding
The funding was provided by Medical College of Wisconsin Division of General Surgery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) and the hospitals participating in the ACS-NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Disclosures
Dr. Jon Gould is a consultant for Torax Medical. Tammy Kindel, Rana Higgins, Kate Lak, Alexander Nielsen, Melissa Helm, and Zachary Helmen have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Nielsen, A.W., Helm, M.C., Kindel, T. et al. Perioperative bleeding and blood transfusion are major risk factors for venous thromboembolism following bariatric surgery. Surg Endosc 32, 2488–2495 (2018). https://doi.org/10.1007/s00464-017-5951-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5951-9