Abstract
Introduction
Previous data demonstrate that patients who receive bariatric surgery at a Center of Excellence are different than those who receive care at non-accredited centers. Canada provides a unique opportunity to naturally exclude confounders such as insurance status, hospital ownership, and lack of access on comparisons between hospitals and surgeons in bariatric surgery outcomes. The objective of this study was to determine the effect of hospital accreditation and other health system factors on all-cause morbidity after bariatric surgery in Canada.
Methods
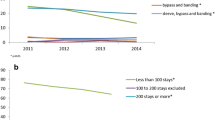
This was a population-based study of all patients aged ≥18 who received a bariatric procedure in Canada (excluding Quebec) from April 2008 until March 2015. The main outcomes for this study were all-cause morbidity and costs during the index admission. All-cause morbidity included any documented complication which extended length of stay by 24 h or required reoperation. Risk-adjusted hierarchical regression models were used to determine predictors of morbidity and cost.
Results
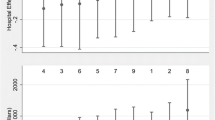
Overall, 18,398 patients were identified and the all-cause morbidity rate was 10.1%. Surgeon volume and teaching hospitals were both found to significantly decrease the odds of all-cause morbidity. Specifically, for each increase in 25 bariatric cases per year, the odds of all-cause morbidity was 0.94 times lower (95% CI 0.87–1.00, p = 0.03). Teaching hospitals conferred a 0.75 lower odds of all-cause morbidity (95% CI 0.58–0.95, p < 0.001). Importantly, formal accreditation was not associated with a decrease in all-cause morbidity within a universal healthcare system. No health system factors were associated with significant cost differences.
Conclusion
This national cohort study found that surgeon volume and teaching hospitals predicted lower all-cause morbidity after surgery while hospital accreditation was not a significant factor.
Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25:1822–1832
Sharma AM (2016) Inequalities in access to bariatric surgery in Canada. CMAJ 188:317–318
Canadian Institute for Health Information (2014) Bariatric Surgery in Canada
Saleh F, Doumouras AG, Gmora S, Anvari M, Hong D (2016) Outcomes of the Ontario Bariatric Network: a cohort study. Can Med Assoc J Open 4:E383–E389
Telem DA, Talamini M, Altieri M, Yang J, Zhang Q, Pryor AD (2015) The effect of national hospital accreditation in bariatric surgery on perioperative outcomes and long-term mortality. Surg Obes Relat Dis 11:749–757
Morton JM, Garg T, Nguyen N (2014) Does hospital accreditation impact bariatric surgery safety? Ann Surg 260:504-8-9
Celio AC, Kasten KR, Brinkley J, Chung AY, Burruss MB, Pories WJ, Spaniolas K (2016) Effect of surgeon volume on sleeve gastrectomy outcomes. Obes Surg 26:2700–2704
Yang YT, Pomeranz JL (2012) States variations in the provision of bariatric surgery under affordable care act exchanges. Surg Obes Relat Dis 11:715–720
Bhogal SK, Reddigan JI, Rotstein OD, Cohen A, Glockler D, Tricco AC, Smylie JK, Glazer SA, Pennington J, Conn LG, Jackson TD (2015) Inequity to the utilization of bariatric surgery: a systematic review and meta-analysis. Obes Surg 25:888–899
Martin M, Beekley A, Kjorstad R, Sebesta J (2005) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis 6:8–15
Pickett-Blakely OE, Huizinga MM, Clark JM (2012) Sociodemographic trends in bariatric surgery utilization in the USA. Obes Surg 22:838–842
Doumouras AG, Saleh F, Gmora S, Anvari M, Hong D (2016) Regional variations in the public delivery of bariatric surgery: an evaluation of the center of excellence model. Ann Surg 263:306–311
Dallal RM, Trang A (2012) Analysis of perioperative outcomes, length of hospital stay, and readmission rate after gastric bypass. Surg Endosc Other Interv Tech 26:754–758
Jensen-Otsu E, Ward EK, Mitchell B, Schoen JA, Rothchild K, Mitchell NS, Austin GL (2014) The effect of medicaid status on weight loss, hospital length of stay, and 30-day readmission after laparoscopic Roux-en-Y gastric bypass surgery. Obes Surg 25:295–301
Grenda TR, Pradarelli JC, Thumma JR, Dimick JB (2015) Variation in hospital episode costs with bariatric surgery. JAMA Surg 150:1109–1115
Lee DS, Stitt A, Wang X, Yu JS, Gurevich Y, Kingsbury KJ, Austin PC, Tu JV (2013) Administrative hospitalization database validation of cardiac procedure codes. Med Care 51:e22–e26
Canadian Institute for Health Information (2011) Data quality documentation, hospital morbidity database, 2010–2011—executive summary. CIHI, Ottawa
Dimick JB, Birkmeyer NJ, Finks JF, Share DA, English WJ, Carlin AM, Birkmeyer JD (2014) Composite measures for profiling hospitals on bariatric surgery performance. JAMA Surg 149:10–16
Canadian Institute for Health Information (2011) Canadian MIS database—hospital financial performance indicators, 1999–2000 to 2009–2010, methodological notes, Revised August 2011. CIHI, Ottawa
Lawson EH, Ko CY, Adams JL, Chow WB, Hall BL (2013) Reliability of evaluating hospital quality by colorectal surgical site infection type. Ann Surg 258:994–1000
Shih T, Cole AI, Al-Attar PM, Chakrabarti A, Fardous HA, Helvie PF, Kemp MT, Lee C, Shtull-Leber E, Campbell DAJ, Englesbe MJ (2015) Reliability of surgeon-specific reporting of complications after colectomy. Ann Surg 261:920–925
Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, Wang X, Liu Y, Kraemer K, Meng X, Merkow R, Chow W, Matel B, Richards K, Hart AJ, Dimick JB, Hall BL (2013) Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 217(336–346):e1
Padwal R, Klarenbach S, Wiebe N, Hazel M, Birch D, Karmali S, Sharma AM, Manns B, Tonelli M (2011) Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med 26:1183–1194
Smith MD, Patterson E, Wahed AS, Belle SH, Bessler M, Courcoulas AP, Flum D, Halpin V, Mitchell JE, Pomp A, Pories WJ, Wolfe B (2010) Relationship between surgeon volume and adverse outcomes after RYGB in Longitudinal Assessment of Bariatric Surgery (LABS) study. Surg Obes Relat Dis 6:118–125
Hollenbeak CS, Rogers AM, Barrus B, Wadiwala I, Cooney RN (2008) Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery 144:736–743
Weller WE, Hannan EL (2006) Relationship between provider volume and postoperative complications for bariatric procedures in New York state. J Am Coll Surg 202:753–761
Birkmeyer NJO, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD (2010) Hospital complication rates with bariatric surgery in Michigan. JAMA 304:435–442
Zevin B, Aggarwal R, Grantcharov TP (2012) Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 256:60–71
Carbonell AM, Lincourt AE, Matthews BD, Kercher KW, Sing RF, Heniford BT (2005) National study of the effect of patient and hospital characteristics on bariatric surgery outcomes. Am Surg 71:308–314
Kohn GP, Galanko JA, Overby DW, Farrell TM (2010) High case volumes and surgical fellowships are associated with improved outcomes for bariatric surgery patients: a justification of current credentialing initiatives for practice and training. J Am Coll Surg 210:909–918
Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE (2004) The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg 240:586–93–4
Jafari MD, Jafari F, Young MT, Smith BR, Phalen MJ, Nguyen NT (2013) Volume and outcome relationship in bariatric surgery in the laparoscopic era. Surg Endosc 27:4539–4546
Dimick JB, Nicholas LH, Ryan AM, Thumma JR, Birkmeyer JD (2013) Bariatric surgery complications before vs after implementation of a national policy restricting coverage to centers of excellence. JAMA 309:792–799
Nguyen NT, Hohmann S, Slone J, Varela E, Smith BR, Hoyt D (2010) Improved bariatric surgery outcomes for Medicare beneficiaries after implementation of the medicare national coverage determination. Arch Surg 145:72–78
Livingston EH (2009) Bariatric surgery outcomes at designated centers of excellence vs nondesignated programs. Arch Surg 144:319–325 (discussion 325)
Flum DR, Kwon S, MacLeod K, Wang B, Alfonso-Cristancho R, Garrison LP, Sullivan SD, Collaborative Bariatric Obesity Outcome Modeling (2011) The use, safety and cost of bariatric surgery before and after Medicareʼs National Coverage decision. Ann Surg 254:860–865
Varban OA, Reames BN, Finks JF, Thumma JR, Dimick JB (2010) Hospital volume and outcomes for laparoscopic gastric bypass and adjustable gastric banding in the modern era. Surg Obes Relat Dis 11:343–349
Kim PS, Telem DA, Altieri MS, Talamini M, Yang J, Zhang Q, Pryor AD (2015) Bariatric outcomes are significantly improved in hospitals with fellowship council-accredited bariatric fellowships. J Gastrointest Surg 19:594–597
Dimick JB, Cowan JA, Colletti LM, Upchurch GR (2004) Hospital teaching status and outcomes of complex surgical procedures in the United States. Arch Surg 139:137
Livingston EH, Burchell I (2010) Reduced access to care resulting from centers of excellence initiatives in bariatric surgery. Arch Surg 145:993
Doumouras AG, Saleh F, Anvari S, Gmora S, Anvari M, Hong D (2017) Mastery in bariatric surgery: the long-term surgeon learning curve of Roux-en-Y gastric bypass. Ann Surg. doi:10.1097/SLA.0000000000002180 (Epub ahead of print)
Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, Hauri D, Graf R, Clavien P-A (2011) The impact of complications on costs of major surgical procedures. Ann Surg 254:907–913
Doumouras AG, Saleh F, Tarride J-E, Hong D (2016) A population-based analysis of the drivers of short-term costs after bariatric surgery within a publicly funded regionalized center of excellence system. Surg Obes Relat Dis 12:1023–1031
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Doumouras, Saleh, Gmora, Hong, Anvari, and Ms. Anvari have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Doumouras, A.G., Saleh, F., Anvari, S. et al. The effect of health system factors on outcomes and costs after bariatric surgery in a universal healthcare system: a national cohort study of bariatric surgery in Canada. Surg Endosc 31, 4816–4823 (2017). https://doi.org/10.1007/s00464-017-5559-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5559-0