Abstract
Background
The issue of mesh fixation in endoscopic inguinal hernia repair is frequently debated and still no conclusive data exist on differences between methods regarding long-term outcome and postoperative complications. The quantity of trials and the simultaneous lack of high-quality evidence raise the question how future trials should be planned.
Methods
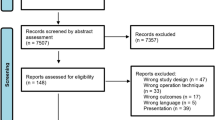
PubMed, EMBASE and the Cochrane Library were searched, using the filters “randomised clinical trials” and “humans”. Trials that compared one method of mesh fixation with another fixation method or with non-fixation in endoscopic inguinal hernia repair were eligible. To be included, the trial was required to have assessed at least one of the following primary outcome parameters: recurrence; surgical site infection; chronic pain; or quality-of-life.
Results
Fourteen trials assessing 2161 patients and 2562 hernia repairs were included. Only two trials were rated as low risk for bias. Eight trials evaluated recurrence or surgical site infection; none of these could show significant differences between methods of fixation. Two of 11 trials assessing chronic pain described significant differences between methods of fixation. One of two trials evaluating quality-of-life showed significant differences between fixation methods in certain functions.
Conclusion
High-quality evidence for differences between the assessed mesh fixation techniques is still lacking. From a socioeconomic and ethical point of view, it is necessary that future trials will be properly designed. As small- and medium-sized single-centre trials have proven unable to find answers, register studies or multi-centre studies with an evident focus on methodology and study design are needed in order to answer questions about mesh fixation in inguinal hernia repair.

Similar content being viewed by others
References
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. doi:10.1007/s10029-009-0529-7
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18:151–163. doi:10.1007/s10029-014-1236-6
Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Grimes KL, Klinge U, Kockerling F, Koeckerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P, International Endohernia Society (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29:289–321. doi:10.1007/s00464-014-3917-8
Antoniou SA, Köhler G, Antoniou GA, Muysoms FE, Pointner R, Granderath F-A (2015) Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg. doi:10.1016/j.amjsurg.2015.06.008
Sajid MS, Ladwa N, Kalra L, McFall M, Baig MK, Sains P (2013) A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 206:103–111. doi:10.1016/j.amjsurg.2012.09.003
Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25:2849–2858. doi:10.1007/s00464-011-1668-3
Shah NS, Fullwood C, Siriwardena AK, Sheen AJ (2014) Mesh fixation at laparoscopic inguinal hernia repair: a meta-analysis comparing tissue glue and tack fixation. World J Surg 38:2558–2570. doi:10.1007/s00268-014-2547-6
Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26:1269–1278. doi:10.1007/s00464-011-2025-2
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 6 :b2700
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928–d5928. doi:10.1136/bmj.d5928
Lederhuber H, Stiede F, Axer S, Dahlstrand U (2015) Evidence assessing mesh fixation in endoscopic inguinal hernia repair: a systematic review. PROSPERO 2015: CRD42015015317. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015015317
Higgins JPT, Green S (2011) Cochrane Handbook for systematic reviews of Interventions. Wiley, New York
Boldo E, Armelles A, Perez de Lucia G, Martin F, Aracil JP, Miralles JM, Martinez D, Escrig J (2008) Pain after laparascopic bilateral hernioplasty : Early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 22:1206–1209. doi:10.1007/s00464-007-9587-z
Koch CA, Greenlee SM, Larson DR, Harrington JR, Farley DR (2006) Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS 10:457–460
Kleidari B, Mahmoudieh M, Yaribakht M, Homaei Z (2014) Mesh fixation in TAPP laparoscopic hernia repair: introduction of a new method in a prospective randomized trial. Surg Endosc 28:531–536. doi:10.1007/s00464-013-3198-7
Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, Redl H, Glaser KS (2012) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254. doi:10.1007/s00464-011-1862-3
Leibl BJ, Kraft B, Redecke JD, Schmedt CG, Ulrich M, Kraft K, Bittner R (2002) Are postoperative complaints and complications influenced by different techniques in fashioning and fixing the mesh in transperitoneal laparoscopic hernioplasty? Results of a prospective randomized trial. World J Surg 26:1481–1484. doi:10.1007/s00268-002-6204-0
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22:757–762. doi:10.1007/s00464-007-9510-7
Chan MS, Melissa CS, Teoh AYB, Bun TAY, Chan KW, Wing CK, Tang YC, Chung TY, Ng EKW, Wai NEK, Leong HT, Tat LH (2014) Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 259:432–437. doi:10.1097/SLA.0b013e3182a6c513
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231. doi:10.1097/01.sla.0000245832.59478.c6
Ferzli GS, Frezza EE, Pecoraro AM, Ahern KD (1999) Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg 188:461–465
Parshad R, Kumar R, Hazrah P, Bal S (2005) A randomized comparison of the early outcome of stapled and unstapled techniques of laparoscopic total extraperitoneal inguinal hernia repair. JSLS 9:403–407
Garg P, Nair S, Shereef M, Thakur JD, Nain N, Menon GR, Ismail M (2011) Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc 25:3300–3306. doi:10.1007/s00464-011-1708-z
Smith AI, Royston CM, Sedman PC (1999) Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. A prospective randomized trial. Surg Endosc 13:804–806
Cambal M, Zonca P, Hrbaty B (2012) Comparison of self-gripping mesh with mesh fixation with fibrin-glue in laparoscopic hernia repair (TAPP). Bratisl Lek Listy 113:103–107
Moreno-Egea A, Torralba Martínez JA, Morales Cuenca G, Aguayo Albasini JL (2004) Randomized clinical trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg 139:1376–1379. doi:10.1001/archsurg.139.12.1376
Rutkow IM, Robbins AW (1993) Demographic, classification, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73:413–426
Nyhus LM, Klein MS, Rogers FB (1991) Inguinal hernia. Curr Probl Surg 28:401–450
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T, CONSORT GROUP (Consolidated Standards of Reporting Trials) (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134:663–694
Halpern SD, Karlawish JHT, Berlin JA (2002) The continuing unethical conduct of underpowered clinical trials. JAMA 288:358–362
Mayer F, Niebuhr H, Lechner M, Dinnewitzer A, Köhler G, Hukauf M, Fortelny RH, Bittner R, Kockerling F (2016) When is mesh fixation in TAPP-repair of primary inguinal hernia repair necessary? The register-based analysis of 11,230 cases. Surg Endosc 30:4363–4371. doi:10.1007/s00464-016-4754-8
Gutlic N, Rogmark P, Nordin P, Petersson U, Montgomery A (2016) Impact of mesh fixation on chronic pain in total extraperitoneal inguinal hernia repair (TEP): a nationwide register-based study. Ann Surg 263:1199–1206. doi:10.1097/SLA.0000000000001306
Farrar JT (2010) Advances in clinical research methodology for pain clinical trials. Nat Med 16:1284–1293. doi:10.1038/nm.2249
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EKB, Kvarstein G, Stubhaug A (2008) Assessment of pain. Br J Anaesth 101:17–24. doi:10.1093/bja/aen103
Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J, IMMPACT (2005) Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113: 9–19
Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB, Cleeland C, Dionne R, Farrar JT, Galer BS, Hewitt DJ, Jadad AR, Katz NP, Kramer LD, Manning DC, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robinson JP, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Witter J (2003) Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain 106:337–345
Helms PJ (2002) “Real world” pragmatic clinical trials: what are they and what do they tell us? Pediatr Allergy Immunol 13:4–9
Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS (2006) Criteria for distinguishing effectiveness from efficacy trials in systematic reviews. Technical Reviews, No. 12. Agency for Healthcare Research and Quality (US), Rockville (MD). https://www.ncbi.nlm.nih.gov/books/NBK44029/
MacRae KD (1989) Pragmatic versus explanatory trials. Int J Technol Assess Health Care 5:333–339
Williams HC, Burden-Teh E, Nunn AJ (2015) What is a pragmatic clinical trial? J Invest Dermatol 135:e33. doi:10.1038/jid.2015.134
Acknowledgements
The authors would like to thank Thomas Hallgren MD, PhD and Simon Agerskov MD for proofreading the article and providing language corrections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hans Lederhuber holds a grant from the Swedish Society for Surgical Innovation (SIKT), founded by BARD Norden. The grant has no connection to the submitted work. Franziska Stiede, Stephan Axer and Ursula Dahlstrand have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lederhuber, H., Stiede, F., Axer, S. et al. Mesh fixation in endoscopic inguinal hernia repair: evaluation of methodology based on a systematic review of randomised clinical trials. Surg Endosc 31, 4370–4381 (2017). https://doi.org/10.1007/s00464-017-5509-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5509-x