Abstract
Objectives
The aim of this study was to compare the effect of transabdominal preperitoneal (TAPP) inguinal hernioplasty with or without mesh fixation on chronic pain and quality of life of patients.
Methods
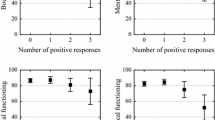
One hundred patients with a simple oblique inguinal hernia were included and treated at the Second Affiliated Hospital of Kunming Medical University from July of 2015 to July of 2016. Patients were randomly assigned to TAPP inguinal hernioplasty with mesh fixation (fixation group, n = 50) or without mesh fixation (non-fixation group, n = 50). Observation indices such as mean operative time, time to ambulation, hospitalization expense, and complications were recorded. The visual analog scale (VAS) was adopted for pain evaluation 2 days, 3 months, and 6 months postoperatively. The 36-item short-form health survey (SF-36) was adopted for life quality scoring 3 months postoperatively.
Results
No recurrence or incisional infections were observed during follow-up in either group. The mean operative time, time to ambulation, and hospitalization expense of the non-fixation group were all significantly reduced compared to those of the fixation group. The VAS score 2 days, 3 months, and 6 months postoperatively of the non-fixation group were significantly lower than in the fixation group. The physical function, role physical, bodily pain, and general health in the non-fixation group were each significantly higher than in the fixation group. In contrast, vitality, social function, role emotional, and mental health showed no significant differences across groups.
Conclusions
For patients with primary unilateral oblique inguinal hernia with a defect size less than 4.0 cm in diameter, TAPP inguinal hernioplasty without mesh fixation was safe and effective. Furthermore, this shortened the operative time, promoted early ambulation, decreased hospitalization expenses, alleviated postoperative pain, and improved quality of life.
Similar content being viewed by others
References
Shulman AG, Amid PK, Lichtenstein IL (1992) The safety of mesh repair for primary inguinal hernias: results of 3019 operations from five diverse surgical sources. Am Surg 58(4):255–257
Douek M, Smith G, Oshowo A, Stoker DL, Wellwood JM (2003) Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ 326(7397):1012–1013
Palmqvist E, Larsson K, Anell A, Hjalmarsson C (2013) Prospective study of pain, quality of life and the economic impact of open inguinal hernia repair. Br J Surg 100(11):1483–1488. doi:10.1002/bjs.9232
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after Mesh-repair of inguinal hernia:a systematic review. Am J Surg 194(3):394–400. doi:10.1016/j.amjsurg.2007.02.012
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219. doi:10.1097/01.sla.0000218081.53940.01
Sajid MS, Ladwa N, Kalra L, Hutson K, Sains P, Baig MK (2012) A meta-analysis examining the use of tacker fixation versus no-fixation of mesh in laparoscopic inguinal hernia repair. Int J Surg 10(5):231. doi:10.1016/j.ijsu.2012.03.001
Lovisetto F, Zonta S, Rota E et al (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245(2):222–231. doi:10.1097/01.sla.0000245832.59478.c6
Alfieri S, Di Miceli D, Doglietto GB (2007) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair. Ann Surg 245(4):663. doi:10.1097/01.sla.0000259048.32440.5b
Perneger TV, Leplège A, Etter JF, Rougemont A (1995) Validation of a French-language version of the MOS 36-item short form health survey (SF-36) in young healthy adults. J Clin Epidemiol 48(8):1051–1160
Loos MJ, Roumen RM, Scheltinga MR (2007) Chronic sequelae of common elective groin hernia repair. Hernia 11(2):169–173. doi:10.1007/s10029-007-0196-5
Koning GG, Andeweg CS, Keus F et al (2012) The transrectus sheath preperitoneal mesh repair for inguinal hernia: technique, rationale, and results of the first 50 cases. Hernia 16(3):299. doi:10.1007/s10029-011-0893-y
McCarthy M Jr, Chang CH, Pickard AS et al (2005) Visual analog scales for assessing surgical pain. J Am Coll Surg 201(2):245–252. doi:10.1016/j.jamcollsurg.2005.03.034
Stewart AL, Hays RD, Ware JE Jr (1988) The MOS short form General Health Survey: reliability and validity in a patient population. Med Care 26(7):735
Bittner R, Arregui ME, Bisgaard T, et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843. doi:10.1007/s00464-011-1799-6.
Bittner R, Montgomery MA, Arregui E et al (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29(2):289–321. doi:10.1007/s00464-014-3917-8
Acknowledgements
The authors are thankful to the Second Affiliated Hospital of Kunming Medical University for the management of our inguinal hernia patient database. This work was supported by the Wu Jieping Medical Foundation of China (No. 320.6750.16211).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Weiming Li, Dali Sun, Yanbo Sun, Yunyun Cen, Shumin Li, Qingwen Xu, Yijun Li, Yuxing Qi, Yueying Lin, Ting Yang, and Pengyuan Xu have no conflicts of interest or financial ties to disclose.
Additional information
Weiming Li and Dali Sun have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, W., Sun, D., Sun, Y. et al. The effect of transabdominal preperitoneal (TAPP) inguinal hernioplasty on chronic pain and quality of life of patients: mesh fixation versus non-fixation. Surg Endosc 31, 4238–4243 (2017). https://doi.org/10.1007/s00464-017-5485-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5485-1