Abstract
Background
Minimally invasive esophagectomy (MIE) has been shown to be a feasible technique for the treatment of esophageal cancer; however, its postoperative morbidity remains high. This retrospective study aimed to evaluate the effect of postoperative complications on long-term outcomes in patients who have undergone MIE for esophageal squamous cell carcinoma (ESCC).
Methods
This retrospective study enrolled patients who had undergone MIE for ESCC between September 2009 and November 2014; all procedures were performed by a single surgical team. Relevant patient characteristics and postoperative variables were collected and evaluated. The disease-free survival (DFS) and disease-specific survival (DSS) were determined by the Kaplan–Meier method, and compared by log-rank tests. Possible predictors of survival were subjected to univariate analysis and multivariate Cox proportional hazard regression analysis.
Results
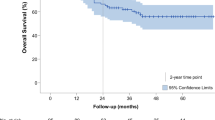
In all, data on 214 patients with ESCC were analyzed, including 170 men and 44 women. All study subjects had undergone thoracoscopic or thoracoscopic–laparoscopic esophagectomy and cervical esophagogastric anastomosis. One hundred and thirty patients (60.7%) had postoperative complications (Grades 1–4). The overall DFS and DSS rates were 80.0 and 88.9% at 1 year, 48.6 and 54.2% at 3 years, and 43.2 and 43.5% at 5 years, respectively. Univariate analysis and multivariate Cox proportional hazard regression analysis showed that T stage, N stage, and tumor grade were independent prognostic factors for long-term survival; however, postoperative complications had no significant effect on the DFS or DSS of this patient cohort (log-rank test, p = 0.354 and 0.160, respectively).
Conclusions
Postoperative complications have no significant effect on long-term survival in patients who have undergone MIE for ESCC.


Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey SM, Dong ZW, Mark SD, Qiao YL, Taylor PR (2005) Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in China. Int J Cancer 113:456–463
Ajani JA (2013) NCCN clinical practice guidelines in oncology, esophageal and esophagogastric junction cancers, v.2.2013. http://www.nccn.org. Accessed 23 July 2013
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37:7–11
Dolan JP, Kaur T, Diggs BS, Luna RA, Schipper PH, Tieu BH, Sheppard BC, Hunter JG (2013) Impact of comorbidity on outcomes and overall survival after open and minimally invasive esophagectomy for locally advanced esophageal cancer. Surg Endosc 27:4094–4103
Osugi H, Takemura M, Higashino M, Takada N, Lee S, Kinoshita H (2003) A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113
Palazzo F, Rosato EL, Chaudhary A, Evans NR, Sendecki JA, Keith S, Chojnacki KA, Yeo CJ, Berger AC (2015) Minimally invasive esophagectomy provides significant survival advantage compared with open or hybrid esophagectomy for patients with cancers of the esophagus and gastroesophageal junction. J Am Coll Surg 220:672–679
Lindner K, Fritz M, Haane C, Senninger N, Palmes D, Hummel R (2014) Postoperative complications do not affect long-term outcome in esophageal cancer patients. World J Surg 38:2652–2661
Xia BT, Rosato EL, Chojnacki KA, Crawford AG, Wekster B, Berger AC (2013) Major perioperative morbidity does not affect long-term survival in patients undergoing esophagectomy for cancer of the esophagus or gastroesophageal junction. World J Surg 37:408–415
Lerut T, Moons J, Coosemans W, Van Raemdonck D, De Leyn P, Decaluwé H, Decker G, Nafteux P (2009) Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg 250:798–807
Luc G, Durand M, Chiche L, Collet D (2015) Major post-operative complications predict long-term survival after esophagectomy in patients with adenocarcinoma of the esophagus. World J Surg 39:216–222
Rice TW, Blackstone EH, Rusch VW (2010) 7th edition of the AJCC Cancer staging manual: esophagus and esophagogastric junction. Ann Surg Oncol 17:1721–1724
Guo W, Zhao YP, Jiang YG, Niu HJ, Liu XH, Ma Z, Wang RW (2012) Prevention of postoperative chylothoraxwith thoracic duct ligation during video-assisted thoracoscopic esophagectomy for cancer. Surg Endosc 26:1332–1336
Deng B, Tan QY, Jiang YG, Zhao YP, Zhou JH, Chen GC, Wang RW (2010) Prevention of early delayed gastric emptying after high-level esophagogastrostomy by pyloric digital fracture. World J Surg 34:2837–2843
Guo W, Zou YB, Ma Z, Niu HJ, Jiang YG, Zhao YP, Gong TQ, Wang RW (2013) One surgeon’s learning curve for video-assisted thoracoscopic esophagectomy for esophageal cancer with the patient in lateral positon: how many cases are needed to reach competence? Surg Endosc 27:1346–1352
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Ninomiya I, Okamoto K, Fujimura T, Fushida S, Osugi H, Ohta T (2014) Oncologic outcomes of thoracoscopic esophagectomy with extended lymph node dissection: 10-year experience from a single center. World J Surg 38:120–130
Puntambekar SP, Agarwal GA, Joshi SN, Rayate NV, Sathe RM, Patil AM (2010) Thoracolaparoscopy in the lateral position for esophageal cancer: the experience of a single institution with 112 consecutive patients. Surg Endosc 24:2407–2414
Wang H, Feng M, Tan L, Wang Q (2010) Comparison of the short-term quality of life in patients with esophageal cancer after subtotal esophagectomy via video-assisted thoracoscopic or open surgery. Dis Esophagus 23:408–414
Dindo D, Clavien PA (2008) What is a surgical complication? World J Surg 32:939–941
Smithers BM, Gotley DC, Martin I, Thomas JM (2007) Comparison of the outcomes between open and minimally invasive esophagectomy. Ann Surg 245:232–240
Burdall OC, Boddy AP, Fullick J, Blazeby J, Krysztopik R, Streets C, Hollowood A, Barham CP, Titcomb D (2015) A comparative study of survival after minimally invasive and open oesophagectomy. Surg Endosc 29:431–437
DerHagopian RP, Sugarbaker EV, Ketcham A (1978) Inflammatory oncotaxis. JAMA 240:374–375
Scarpa M, Cavallin F, Saadeh LM, Pinto E, Alfieri R, Cagol M, Da Roit A, Pizzolato E, Noaro G, Pozza G, Castoro C (2015) Hybrid minimally invasive esophagectomy for cancer: impact on postoperative inflammatory and nutritional status. Dis Esophagus. doi:10.1111/dote.12418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kun-Kun Li, Yin-Jian Wang, Xue-Hai Liu, Qun-You Tan, Yao-Guang Jiang, and Wei Guo have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Li, KK., Wang, YJ., Liu, XH. et al. The effect of postoperative complications on survival of patients after minimally invasive esophagectomy for esophageal cancer. Surg Endosc 31, 3475–3482 (2017). https://doi.org/10.1007/s00464-016-5372-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5372-1