Abstract
Background
To investigate the incidence of and factors associated with postoperative complications and failure to rescue following laparoscopic and open gastrectomy for gastric cancer.
Study design
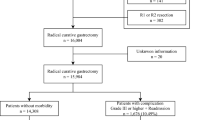
We analyzed the records of 4124 patients who underwent a laparoscopic or open gastrectomy for gastric cancer. One-to-one propensity score matching was performed to compare the difference between the two groups.
Results
A total of 4124 patients were included in the study, 627 of whom (15.2 %) developed postoperative complications. Postoperative deaths occurred in 23 (0.6 %) patients with serious complications. In the propensity score matching analysis with 1361 pairs, no significant differences in the rates of overall complications (14.2 vs. 16.5 %, p = 0.093) were observed between laparoscopic and open gastrectomy group. In-hospital mortality decreased in patients who underwent laparoscopic gastrectomy compared to patients who underwent open gastrectomy (0.3 vs. 1.2 %, p = 0.004). Failure to rescue rates were lower in patients who underwent laparoscopic gastrectomy (2.1 vs. 7.6 %, p = 0.008). Multivariate analysis showed that older age, tumor location, TNM stage classification, extent of gastric resection, operative time and intra-operative blood loss were adverse risk factors for postoperative complications. Laparoscopic gastrectomy was found to be a protective factor for failure to rescue. Complications associated with failure to rescue included abdominal bleeding, anastomotic leakage and cardiac events. In-hospital mortality increased as the number of complications per patient increased.
Conclusions
Assuming equal competence with open and laparoscopic approaches of a surgeon, the proportion of patients with postoperative complications were similar among those who underwent laparoscopic gastrectomy compared to patients who underwent open gastrectomy. However, when complications occurred, patients with open gastrectomy were more likely to die.


Similar content being viewed by others
References
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N, Japanese Laparoscopic Surgery Study Group (2007) A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg 245(1):68–72
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 241(2):232–237
Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, Ryu SW, Lee HJ, Song KY (2010) Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg 251:417–420
Raval MV, Hamilton BH, Ko CY, Hall BL (2011) The importance of assessing both inpatient and outpatient surgical quality. Ann Surg 253:611–618
Dimick JB, Staiger DO, Hall BL, Ko CY, Birkmeyer JD (2013) Composite measures for profiling hospitals on surgical morbidity. Ann Surg 257:67–72
Birkmeyer JD, Dimick JB, Birkmeyer NJ (2004) Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg 198:626–632
Silber JH, Rosenbaum PR, Schwartz JS, Ross RN, Williams SV (1995) Evaluation of the complication rate as a measure of quality of care in coronary artery bypass graft surgery. JAMA 274(4):317–323
Silber JH, Rosenbaum PR, Williams SV, Ross RN, Schwartz JS (1997) The relationship between choice of outcome measure and hospital rank in general surgical procedures: implications for quality assessment. Int J Qual Health Care 9(3):193–200
Almoudaris AM, Burns EM, Bottle A, Aylin P, Darzi A, Vincent C, Faiz O (2013) Single measures of performance do not reflect overall institutional quality in colorectal cancer surgery. Gut 62(3):423–429
Wright JD, Ananth CV, Ojalvo L, Herzog TJ, Lewin SN, Lu YS, Neugut AI, Hershman DL (2013) Failure to rescue after major gynecologic surgery. Am J Obstet Gynecol 209(5):420.e421–420.e428
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg 250:1029–1034
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Variation in hospital mortality associated with inpatient surgery. N Engl J Med 361:1368–1375
Ghaferi AA, Birkmeyer JD, Dimick JB (2011) Hospital volume and failure to rescue with high-risk surgery. Med Care 49:1076–1081
Pasquali SK, He X, Jacobs JP, Jacobs ML, O’Brien SM, Gaynor JW (2012) Evaluation of failure to rescue as a quality metric in pediatric heart surgery: an analysis of the STS Congenital Heart Surgery Database. Ann Thorac Surg 94:573–580
Wright JD, Herzog TJ, Siddiq Z, Arend R, Neugut AI, Burke WM, Lewin SN, Ananth CV, Hershman DL (2012) Failure to rescue as a source of variation in hospital mortality for ovarian cancer. J Clin Oncol 30:3976–3982
Hu YF, Yu J, Zhang C, Wang YN, Cheng X, Huang F, Li GX (2010) Development and implementation of a clinical data mining system for gastric cancer surgery. Zhonghua Wei Chang Wai Ke Za Zhi 13(7):510–515
Sobin LH, Gospodarowicz MK, Wittekind C (2010) International Union Against Cancer (UICC) TNM classification of malignant tumours, 7th edn. Wiley-Liss, New York
Huang CM, Tu RH, Lin JX, Zheng CH, Li P, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M (2015) A scoring system to predict the risk of postoperative complications after laparoscopic gastrectomy for gastric cancer based on a large-scale retrospective study. Medicine (Baltimore) 94(17):e812
Nakajima T (2002) Gastric cancer treatment guidelines in Japan. Gastric Cancer 5(1):1–5
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Jung MR, Park YK, Seon JW, Kim KY, Cheong O, Ryu SY (2012) Definition and classification of complications of gastrectomy for gastric cancer based on the accordion severity grading system. World J Surg 36(10):2400–2411
Bruce J, Krukowski ZH, Al-Khairy G, Russell EM, Park KG (2001) Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg 88(9):1157–1168
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Orsenigo E, Bissolati M, Socci C, Chiari D, Muffatti F, Nifosi J, Staudacher C (2014) Duodenal stump fistula after gastric surgery for malignancies: a retrospective analysis of risk factors in a single centre experience. Gastric Cancer 17(4):733–744
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13(10):606–608
Assumpcao L, Cameron JL, Wolfgang CL, Edil B, Choti MA, Herman JM, Geschwind JF, Hong K, Georgiades C, Schulick RD, Pawlik TM (2008) Incidence and management of chyle leaks following pancreatic resection: a high volume single-center institutional experience. J Gastrointest Surg 12(11):1915–1923
Holte K, Kehlet H (2000) Postoperative ileus: a preventable event. Br J Surg 87(11):1480–1493
Arozullah AM, Khuri SF, Henderson WG, Daley J, Participants in the National Veterans Affairs Surgical Quality Improvement Program (2001) Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 135(10):847–857
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Tamirisa NP, Parmar AD, Vargas GM, Mehta HB, Kilbane EM, Hall BL, Pitt HA, Riall TS (2016) Relative contributions of complications and failure to rescue on mortality in older patients undergoing pancreatectomy. Ann Surg 263(2):385–391
Yasunaga H, Horiguchi H, Kuwabara K, Matsuda S, Fushimi K, Hashimoto H, Ayanian JZ (2013) Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg 257(4):640–646
Lee JH, Han HS, Lee JH (2005) A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer: early results. Surg Endosc 19:168–173
Guzman EA, Pigazzi A, Lee B, Soriano PA, Nelson RA, Benjamin Paz I, Trisal V, Kim J, Ellenhorn JD (2009) Totally laparoscopic gastric resection with extended lymphadenectomy for gastric adenocarcinoma. Ann Surg Oncol 16:2218–2223
Kim MC, Kim KH, Kim HH, Jung GJ (2005) Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol 91:90–94
Lee JH, Yom CK, Han HS (2009) Comparison of long-term outcomes of laparoscopy-assisted and open distal gastrectomy for early gastric cancer. Surg Endosc 23:1759–1763
Lee SI, Choi YS, Park DJ, Kim HH, Yang HK, Kim MC (2006) Comparative study of laparoscopy-assisted distal gastrectomy and open distal gastrectomy. J Am Coll Surg 202:874–880
Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K (2008) Effect of obesity on technical feasibility and postoperative outcomes of laparoscopy-assisted distal gastrectomy—comparison with open distal gastrectomy. J Gastrointest Surg 12:997–1004
Vinuela EF, Gonen M, Brennan MF, Coit DG, Strong VE (2012) Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg 255:446–456
Quan Y, Huang A, Ye M, Xu M, Zhuang B, Zhang P, Yu B, Min Z (2015) Comparison of laparoscopic versus open gastrectomy for advanced gastric cancer: an updated meta-analysis. Gastric Cancer. doi:10.1007/s10120-015-0516-x
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17(19):2265–2281
Kumagai K, Hiki N, Nunobe S, Jiang X, Kubota T, Aikou S, Tanimura S, Sano T, Yamaguchi T (2014) Potentially fatal complications for elderly patients after laparoscopy-assisted distal gastrectomy. Gastric Cancer 17(3):548–555
Hwang SH, Park DJ, Jee YS, Kim HH, Lee HJ, Yang HK, Lee KU (2009) Risk factors for operative complications in elderly patients during laparoscopy-assisted gastrectomy. J Am Coll Surg 208(2):186–192
Tu RH, Huang CM, Lin JX, Chen QY, Zheng CH, Li P, Xie JW, Wang JB, Lu J, Cao LL, Lin M (2015) A scoring system to predict the risk of organ/space surgical site infections after laparoscopic gastrectomy for gastric cancer based on a large-scale retrospective study. Surg Endosc. doi:10.1007/s00464-015-4594-y
Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, Bonjer HJ, Bemelman WA, Cuesta MA (2012) Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg 255(2):216–221
Shibata J, Ishihara S, Tada N, Kawai K, Tsuno NH, Yamaguchi H, Sunami E, Kitayama J, Watanabe T (2015) Surgical stress response after colorectal resection: a comparison of robotic, laparoscopic, and open surgery. Tech Coloproctol 19(5):275–280
Ferraris VA, Bolanos M, Martin JT, Mahan A, Saha SP (2014) Identification of patients with postoperative complications who are at risk for failure to rescue. JAMA Surg 149(11):1103–1108
Sheetz KH, Krell RW, Englesbe MJ, Birkmeyer JD, Campbell DA Jr, Ghaferi AA (2014) The importance of the first complication: understanding failure to rescue after emergent surgery in the elderly. J Am Coll Surg 219(3):365–370
Gonzalez AA, Dimick JB, Birkmeyer JD, Ghaferi AA (2014) Understanding the volume-outcome effect in cardiovascular surgery: the role of failure to rescue. JAMA Surg 149(2):119–123
Acknowledgments
The authors are thankful to Fujian Medical University Union Hospital for their management of our gastric cancer patient database.
Funding
This study was funded by the National Key Clinical Specialty Discipline Construction program of China (No. [2012]649) and the Key Projects of Science and Technology Plan of Fujian Province (No. 2014Y0025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ru-Hong Tu, Jian-Xian Lin, Chao-Hui Zheng, Ping Li, Jian-Wei Xie, Jia-Bin Wang, Jun Lu, Qi-Yue Chen, Long-Long Cao, Mi Lin and Chang-Ming Huang have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Tu, RH., Lin, JX., Zheng, CH. et al. Complications and failure to rescue following laparoscopic or open gastrectomy for gastric cancer: a propensity-matched analysis. Surg Endosc 31, 2325–2337 (2017). https://doi.org/10.1007/s00464-016-5235-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5235-9