Abstract
Background
While thoracoscopic esophagectomy is a widely performed surgical procedure, only few studies regarding the influence of body position on changes in circulation and breathing, after the surgery, have been reported. This study aimed at evaluating the effect of body position, during surgery, on the postoperative breathing functions of the chest.
Methods
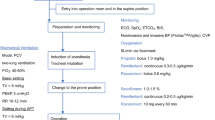
A total of 266 patients who underwent right-sided transthoracic esophagectomy for esophageal cancer from 2004 to 2012 were included in this study. Fifty-four of them underwent open thoracotomies in the left lateral decubitus position (Group O), 108 underwent thoracoscopic esophagectomy in the left lateral decubitus position (Group L) and 104 patients were treated by thoracoscopic esophagectomy in the prone position (Group P). Two patients in Group P, who presented with intra-operative bleeding and underwent thoracotomy, were subsequently excluded from the pulmonary function analysis.
Results
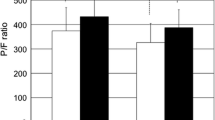
Two patients in Group P had to be changed from the prone position to the lateral decubitus position and underwent thoracotomy in order to control intra-operative bleeding. Despite the significantly longer chest operation period in Group P, total blood loss was significantly lower in this group when compared to Groups O and L. Furthermore, patients in Group P presented with significantly lower water balance during the perioperative period and markedly higher SpO2/FiO2 ratio after the surgery. The incidence of respiratory complications was significantly higher in Group O when compared to the other two groups; however, no significant differences were observed between the Groups L and P.
Conclusion
The findings of this study demonstrate that thoracoscopic esophagectomy in the prone position improves postoperative oxygenation and is therefore a potentially superior surgical approach.

Similar content being viewed by others
References
Morita M, Yoshida R, Ikeda K, Egashira A, Oki E, Sadanaga N, Kakeji Y, Yamanaka T, Maehara Y (2008) Advances in esophageal cancer surgery in Japan: an analysis of 1000 consecutive patients treated at a single institute. Surgery 143(4):499–508
Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y (1994) Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 220:364–372
Fujita H, Kakegawa T, Yamana H, Shima I, Toh Y, Tomita Y, Fujii T, Yamasaki K, Higaki K, Noake T et al (1995) Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 222(5):654–662
Kelsen DP, Ginsberg R, Pajak TF, Sheahan DG, Gunderson L, Mortimer J, Estes N, Haller DG, Ajani J, Kocha W, Minsky BD, Roth JA (1998) Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Eng J Med 339(27):1979–1984
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37(1):7–11
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, Schauer PR, Close JM, Fernando HC (2003) Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238(4):486–494 (discussion 494-495)
Smithers BM, Gotley DC, Martin I, Thomas JM (2007) Comparison of the outcomes between open and minimally invasive esophagectomy. Ann Surg 245(2):232–240
Taguchi S, Osugi H, Higashino M, Tokuhara T, Takada N, Takemura M, Lee S, Kinoshita H (2003) Comparison of three-field esophagectomy for esophageal cancer incorporating open or thoracoscopic thoracotomy. Surg Endosc 17:1445–1450
Cuschieri A (1994) Thoracoscopic subtotal oesophagectomy. Endosc Surg Alliced Technol 2:21–25
Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position—experience of 130 patients. J Am Coll Surg 203(1):7–16
Yatabe T, Kitagawa H, Yamashita K, Akimori T, Hanazaki K, Yokoyama M (2010) Better postoperative oxygenation in thoracoscopic esophagectomy in prone positioning. J Anesth 24(5):803–806
Yatabe T, Kitagawa H, Yamashita K, Hanazaki K, Yokoyama M (2013) Comparison of the perioperative outcome of esophagectomy by thoracoscopy in the prone position with that of thoracotomy in the lateral decubitus position. Surg Today 43(4):386–391
Bonavina L, Laface L, Abate E, Punturieri M, Agosteo E, Nencioni M (2012) Comparison of ventilation and cardiovascular parameters between prone thoracoscopic and Ivor Lewis esophagectomy. Updates Surg 64:81–85
Hale DF, Cannon JW, Batchinsky AI, Cancio LC, Aden JK, White CE, Renz EM, Blackbourne LH, Chung KK (2012) Prone positioning improves oxygenation in adult burn patients with severe acute respiratory distress syndrome. J Trauma Acute Care Surg 72(6):1634–1639
Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, Malacrida R, Di Giulio P, Fumagalli R, Pelosi P, Brazzi L, Latini R (2001) Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med 345(8):568–573
Bajwa AA, Arasi L, Canabal JM, Kramer DJ (2010) Automated prone positioning and axial rotation in critically ill, nontrauma patients with acute respiratory distress syndrome (ARDS). J Intensive Care Med 25(2):121–125
Watanabe I, Fujihara H, Sato K, Ohashi S, Endoh H, Yamakura T, Taga K, Shimoji K (2002) Beneficial effect for patients with hypoxemia after transthoracic esophagectomy. Crit Care Med 30:1799–1802
Pelosi P, Croci M, Calappi E, Cerisara M, Mulazzi D, Vicardi P, Gattinoni L (1995) The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesth Analg 80(5):955–960
Froese AB, Bryan AC (1974) Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 41(3):242–255
Kim DJ, Hyung WJ, Lee CY, Lee JG, Haam SJ, Park IK, Chung KY (2010) Thoracoscopic esophagectomy for esophageal cancer: feasibility and safety of robotic assistance in the prone position. J Thoracoscopic Cardiovasc Surg 139:53–59
Barer GR, Howard P, Shaw JW (1970) Stimulus-response curves for the pulmonary vascular bed to hypoxia and hypercapnia. J Physiol 211(1):139–155
Dorrington KL, Balanos GM, Talbot NP, Robbins PA (2010) Extent to which pulmonary vascular responses to PCO2 and PO2 play a functional role within the healthy human lung. J Appl Physiol 108(5):1084–1096
Pumb B, Talleruphuus U, Christensen NJ, Warberg J, Norsk P (2002) Effect of supine, prone, and lateral positions on cardiovascular and renal variables in human. Am J Physiol Regul Integr Comp Physiol 283(1):R174–R180
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicenter, open-label, randomised control trial. Lancet 379(9829):1887–1892
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Dai Otsubo, Tetsu Nakamura, Masashi Yamamoto, Shingo Kanaji, Kiyonori Kanemitsu, Kimihiro Yamashita, Tatsuya Imanishi, Taro Oshikiri, Yasuo Sumi, Satoshi Suzuki, Daisuke Kuroda and Yoshihiro Kakeji have declared no conflicts of interest associated with this manuscript.
Rights and permissions
About this article
Cite this article
Otsubo, D., Nakamura, T., Yamamoto, M. et al. Prone position in thoracoscopic esophagectomy improves postoperative oxygenation and reduces pulmonary complications. Surg Endosc 31, 1136–1141 (2017). https://doi.org/10.1007/s00464-016-5081-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5081-9