Abstract
Background
Guidelines recommend biologic prosthetics for ventral hernia repair (VHR) in contaminated fields, yet long-term and patient-reported data are limited. We aimed to determine the long-term rate of hernia recurrence, and other clinical and patient-reported outcomes following the use of porcine small intestine submucosa (PSIS) for VHR in a contaminated field.
Methods
Consecutive patients undergoing open VHR with PSIS mesh in a contaminated field from 2004 to 2014 were prospectively evaluated for hernia recurrence and other post-operative complications. Multivariate logistic and Cox regression analyses identified predictors of hernia recurrence and surgical site infection. Patient-reported outcomes were evaluated using SF-36, Hernia-Related Quality-of-Life Survey (HerQLes) and Body Image Questionnaire instruments.
Results
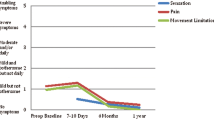
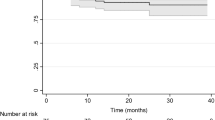
Forty-six hernias were repaired in clean-contaminated [16 (35 %)], contaminated [11 (24 %)] and dirty [19 (41 %)] fields. Median follow-up was 47 months [interquartile range: 31–79] and all patients had greater than 12-month follow-up. Sixteen patients (35 %) were not re-examined. Incidence of surgical site events and surgical site infection were 43 % (n = 20) and 56 % (n = 25), respectively. American Society of Anesthesiologists score 3 or greater was an independent predictor of surgical site infection (odds ratio 5.34 [95 % confidence interval 1.01–41.80], p = 0.04). Hernia recurrence occurred in 61 % (n = 28) with a median time to diagnosis of 16 months [interquartile range 8–26]. After bridged repair, 16 of 18 patients (89 %) recurred, compared to 12 of 28 (43 %) when fascia was approximated (p < 0.01). Bridged repair was an independent predictor of recurrence (odds ratio 10.67 [95 % confidence interval 2.42–76.08], p < 0.01). Patients with recurrences had significantly worse scores on the SF-36 mental health component and self-perceived body image, whereas HerQLes scores were similar.
Conclusions
Hernia recurrences and wound infections are high with the use of biologic PSIS mesh in contaminated surgical fields. Careful consideration is warranted using this approach.

Similar content being viewed by others
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583 discussion 583–575
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
Voyles CR, Richardson JD, Bland KI, Tobin GR, Flint LM, Polk HC Jr (1981) Emergency abdominal wall reconstruction with polypropylene mesh: short-term benefits versus long-term complications. Ann Surg 194:219–223
Jones JW, Jurkovich GJ (1989) Polypropylene mesh closure of infected abdominal wounds. Am Surg 55:73–76
Carbonell AM, Criss CN, Cobb WS, Novitsky YW, Rosen MJ (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 217:991–998
Ventral Hernia Working G, Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF, Rosen M, Silverman RP, Vargo D (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558
Shankaran V, Weber DJ, Reed RL 2nd, Luchette FA (2011) A review of available prosthetics for ventral hernia repair. Ann Surg 253:16–26
Hiles M, Record Ritchie RD, Altizer AM (2009) Are biologic grafts effective for hernia repair?: a systematic review of the literature. Surg Innov 16:26–37
Bachman S, Ramshaw B (2008) Prosthetic material in ventral hernia repair: how do I choose? Surg Clin N Am 88:101–112
Beale EW, Hoxworth RE, Livingston EH, Trussler AP (2012) The role of biologic mesh in abdominal wall reconstruction: a systematic review of the current literature. Am J Surg 204:510–517
Mariette C, Wind P, Micelli Lupinacci R, Tresallet C, Adham M, Arvieux C, Benoist S, Berdah S, Berger A, Briez N, Brigand C, Caiazzo R, Carrere N, Casa C, Collet D, Deguelte S, Dousset B, Dubuisson V, Glehen O, Gineste JC, Hamy A, Lacaine F, Laurent C, Lehur PA, Mabrut JY, Mathieu P, Mathonnet M, Meunier B, Michot F, Ouaissi M, Palot JP, Parc Y, Pattou F, Paye F, Pezet D, Piessen G, Pocard M, Regenet N, Regimbeau JM, Sabbagh C, Zerbib P, Toussaint JM (2014) Practice patterns in complex ventral hernia repair and place of biological grafts: a national survey among French digestive academic surgeons. J Visc Surg 151:9–16
Harth KC, Krpata DM, Chawla A, Blatnik JA, Halaweish I, Rosen MJ (2013) Biologic mesh use practice patterns in abdominal wall reconstruction: a lack of consensus among surgeons. Hernia J Hernias Abdom Wall Surg 17:13–20
Primus FE, Harris HW (2013) A critical review of biologic mesh use in ventral hernia repairs under contaminated conditions. Hernia J Hernias Abdom Wall Surg 17:21–30
Lee L, Mata J, Landry T, Khwaja KA, Vassiliou MC, Fried GM, Feldman LS (2014) A systematic review of synthetic and biologic materials for abdominal wall reinforcement in contaminated fields. Surg Endosc 28:2531–2546
Slater NJ, van der Kolk M, Hendriks T, van Goor H, Bleichrodt RP (2013) Biologic grafts for ventral hernia repair: a systematic review. Am J Surg 205:220–230
Rosen MJ, Krpata DM, Ermlich B, Blatnik JA (2013) A 5-year clinical experience with single-staged repairs of infected and contaminated abdominal wall defects utilizing biologic mesh. Ann Surg 257:991–996
Diaz JJ Jr, Conquest AM, Ferzoco SJ, Vargo D, Miller P, Wu YC, Donahue R (2009) Multi-institutional experience using human acellular dermal matrix for ventral hernia repair in a compromised surgical field. Arch Surg 144:209–215
Urbach DR (2005) Measuring quality of life after surgery. Surg Innov 12:161–165
Brenneman FD, Wright JG, Kennedy ED, McLeod RS (1999) Outcomes research in surgery. World J Surg 23:1220–1223
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Centers for disease control and prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control 27:97–132; quiz 133–134; discussion 196
(1999) Centers for Disease Control and Prevention Guideline for Prevention of Surgical Site Infection. Centers for Disease Control and Prevention
Criss CN, Petro CC, Krpata DM, Seafler CM, Lai N, Fiutem J, Novitsky YW, Rosen MJ (2014) Functional abdominal wall reconstruction improves core physiology and quality-of-life. Surgery 156:176–182
Hiatt EL, Collins RL, Pastorek NJ, Bellows CF (2009) Body image and health locus of control among male patients with incisional hernias. Body image 6:242–245
Sosin M, Patel KM, Albino FP, Nahabedian MY, Bhanot P (2014) A patient-centered appraisal of outcomes following abdominal wall reconstruction: a systematic review of the current literature. Plast Reconstr Surg 133:408–418
Poelman MM, Schellekens JF, Langenhorst BL, Schreurs WH (2010) Health-related quality of life in patients treated for incisional hernia with an onlay technique. Hernia J Hernias Abdom Wall Surg 14:237–242
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc 12:1334–1340
van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF (2012) Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg 204:144–150
Chavarriaga LF, Lin E, Losken A, Cook MW, Jeansonne LO, White BC, Sweeney JF, Galloway JR, Davis SS Jr (2010) Management of complex abdominal wall defects using acellular porcine dermal collagen. Am Surg 76:96–100
Helton WS, Fisichella PM, Berger R, Horgan S, Espat NJ, Abcarian H (2005) Short-term outcomes with small intestinal submucosa for ventral abdominal hernia. Archives of surgery 140:549–560; discussion 560–542
Franklin ME Jr, Trevino JM, Portillo G, Vela I, Glass JL, Gonzalez JJ (2008) The use of porcine small intestinal submucosa as a prosthetic material for laparoscopic hernia repair in infected and potentially contaminated fields: long-term follow-up. Surg Endosc 22:1941–1946
Rogmark P, Petersson U, Bringman S, Ezra E, Osterberg J, Montgomery A (2015) Quality-of-life and Surgical Outcome 1 Year After Open and Laparoscopic Incisional Hernia Repair: PROLOVE: A Randomized Controlled Trial. Annals of surgery
Alaedeen DI, Lipman J, Medalie D, Rosen MJ (2007) The single-staged approach to the surgical management of abdominal wall hernias in contaminated fields. Hernia J Hernias Abdom Wall Surg 11:41–45
Booth JH, Garvey PB, Baumann DP, Selber JC, Nguyen AT, Clemens MW, Liu J, Butler CE (2013) Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. J Am Coll Surg 217:999–1009
Slater NJ, van Goor H, Bleichrodt RP (2015) Large and complex ventral hernia repair using “components separation technique” without mesh results in a high recurrence rate. Am J Surg 209:170–179
Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS, Liang MK (2014) Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy: a systematic review and meta-analysis. JAMA surgery 149:415–421
Acknowledgments
Dr. Amin Madani is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AM is supported by a Quebec Health Science Research (FRQ-S) scholarship and the McGill Surgeon-Scientist Program. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Medtronic.
Disclosures
There was no financial and material support for this work. Drs. Amin Madani, Petru Niculiseanu, Wanda Marini, Pepa A. Kaneva, Benjamin Mappin-Kasirer, Melina Vassiliou, Kosar Khwaja, Paola Fata, Gerald M. Fried and Liane S. Feldman have no conflicts of interest or financial ties to disclose. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Medtronic.
Rights and permissions
About this article
Cite this article
Madani, A., Niculiseanu, P., Marini, W. et al. Biologic mesh for repair of ventral hernias in contaminated fields: long-term clinical and patient-reported outcomes. Surg Endosc 31, 861–871 (2017). https://doi.org/10.1007/s00464-016-5044-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5044-1