Abstract
Background
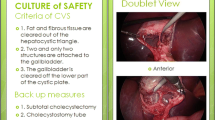
The reported incidence (0.16–1.5 %) of bile duct injury (BDI) during laparoscopic cholecystectomy (LC) is higher than during open cholecystectomy and has not decreased over time despite increasing experience with the procedure. The “critical view of safety” (CVS) technique may help to prevent BDI when certain criteria are met prior to division of any structures. This study aimed to evaluate the adherence of practicing surgeons to the CVS criteria during LC and the impact of a training intervention on CVS identification.
Methods
LC procedures of general surgeons were video-recorded. De-identified recordings were reviewed by a blinded observer and rated on a 6-point scale using the previously published CVS criteria. A coaching program was conducted, and participating surgeons were re-assessed in the same manner.
Results
The observer assessed ten LC videos, each involving a different surgeon. The CVS was adequately achieved by two surgeons (20 %). The remaining eight surgeons (80 %) did not obtain adequate CVS prior to division of any structures, despite two surgeons dictating that they did; the mean score of this group was 1.75. After training, five participating surgeons (50 %) scored > 4, and the mean increased from 1.75 (baseline) to 3.75 (p < 0.05).
Conclusions
The CVS criteria were not routinely used by the majority of participating surgeons. Further, one-fourth of those who claimed to obtain the CVS did so inadequately. All surgeons who participated in training showed improvement during their post-assessment. Our findings suggest that education of practicing surgeons in the application of the CVS during LC can result in increased implementation and quality of the CVS. Pending studies with larger samples, our findings may partly explain the sustained BDI incidence despite increased experience with LC. Our study also supports the value of direct observation of surgical practices and subsequent training for quality improvement.
Similar content being viewed by others
References
Bilimoria KY, Chung J, Soper NJ (2013) Laparoscopic cholecystectomy, intraoperative cholangiograms, and common duct injuries. JAMA 310:801–802
Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M (2011) Critical view of safety during laparoscopic cholecystectomy. JSLS 15:322–325
Soderlund C, Frozanpor F, Linder S (2005) Bile duct injuries at laparoscopic cholecystectomy: a single-institution prospective study. Acute cholecystitis indicates an increased risk. World J Surg 29:987–993
Van de Sande S, Bossens M, Parmentier Y, Gigot JF (2003) National survey on cholecystectomy related bile duct injury–public health and financial aspects in Belgian hospitals–1997. Acta Chir Belg 103:168–180
Krahenbuhl L, Sclabas G, Wente MN, Schafer M, Schlumpf R, Buchler MW (2001) Incidence, risk factors, and prevention of biliary tract injuries during laparoscopic cholecystectomy in Switzerland. World J Surg 25:1325–1330
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus small-incision cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 4:CD006229
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 4:CD006231
Dekker SW, Hugh TB (2008) Laparoscopic bile duct injury: understanding the psychology and heuristics of the error. ANZ J Surg 78:1109–1114
Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, Hunter JG (2003) Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg 237:460–469
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180:101–125
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211:132–138
Sanjay P, Fulke JL, Exon DJ (2010) ‘Critical view of safety’ as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg 14:1280–1284
Nijssen MA, Schreinemakers JM, Meyer Z, van der Schelling GP, Crolla RM, Rijken AM (2015) Complications after laparoscopic cholecystectomy: a video evaluation study of whether the critical view of safety was reached. World J Surg 39:1798–1803
McKinley SK, Brunt LM, Schwaitzberg SD (2014) Prevention of bile duct injury: the case for incorporating educational theories of expertise. Surg Endosc 28:3385–3391
Heistermann HP, Tobusch A, Palmes D (2006) Prevention of bile duct injuries after laparoscopic cholecystectomy. “The critical view of safety”. Zentralbl Chir 131:460–465
Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C (2009) One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg 13:498–503
Sanford DE, Strasberg SM (2014) A simple effective method for generation of a permanent record of the Critical View of Safety during laparoscopic cholecystectomy by intraoperative “doublet” photography. J Am Coll Surg 218:170–178
Emous M, Westerterp M, Wind J, Eerenberg JP, van Geloven AA (2010) Registering the critical view of safety: photo or video? Surg Endosc 24:2527–2530
Yamashita Y, Kimura T, Matsumoto S (2010) A safe laparoscopic cholecystectomy depends upon the establishment of a critical view of safety. Surg Today 40:507–513
Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L (2003) Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA 290:2168–2173
Barbier L, Souche R, Slim K, Ah-Soune P (2014) Long-term consequences of bile duct injury after cholecystectomy. J Visc Surg 151:269–279
Connor S, Garden OJ (2006) Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg 93:158–168
Acknowledgments
Financial support for this study was provided through a Leading Edge Advanced Practice Topics (LEAPT) grant by the Center for Medicare and Medicaid Services.
Authors’ contributions
Stefanidis was involved in study conception and design; Chintalapudi, Tobben, and Pimentel acquired the data; Anderson-Montoya, Oommen, and Stefanidis analyzed and interpreted the data; Chintalapudi, Oommen, and Stefanidis drafted the manuscript; Anderson-Montoya and Stefanidis critically revised the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dimitrios Stefanidis has received honoraria by WL Gore and Davol for teaching and research support by Ethicon Inc. that are unrelated to this project. Bindhu Oommen, Nikita Chintalapudi, Brittany Anderson-Montoya, Daniel Tobben, and Manuel Pimentel have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Stefanidis, D., Chintalapudi, N., Anderson-Montoya, B. et al. How often do surgeons obtain the critical view of safety during laparoscopic cholecystectomy?. Surg Endosc 31, 142–146 (2017). https://doi.org/10.1007/s00464-016-4943-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4943-5