Abstract
Background
Optimization of OR management is a complex problem as each OR has different procedures throughout the day inevitably resulting in scheduling delays, variations in time durations and overall suboptimal performance. There exists a need for a system that automatically tracks procedural progress in real time in the OR. This would allow for efficient monitoring of operating room states and target sources of inefficiency and points of improvement.
Study design
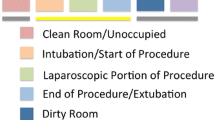
We placed three wireless sensors (floor-mounted pressure sensor, ventilator-mounted bellows motion sensor and ambient light detector, and a general room motion detector) in two ORs at our institution and tracked cases 24 h a day for over 4 months.
Results
We collected data on 238 total cases (107 laparoscopic cases). A total of 176 turnover times were also captured, and we found that the average turnover time between cases was 35 min while the institutional goal was 30 min. Deeper examination showed that 38 % of laparoscopic cases had some aspect of suboptimal activity with the time between extubation and patient exiting the OR being the biggest contributor (16 %).
Conclusion
Our automated system allows for robust, wireless real-time OR monitoring as well as data collection and retrospective data analyses. We plan to continue expanding our system and to project the data in real time for all OR personnel to see. At the same time, we plan on adding key pieces of technology such as RFID and other radio-frequency systems to track patients and physicians to further increase efficiency and patient safety.








Similar content being viewed by others
References
Dexter F, Abouleish AE, Epistein RH, Whitten CW, Lubarsky DA (2003) Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analy 97:1119–1126
Strum DP, Vargas LG, May JH, Bashein G (1997) Surgical suite utilization and capacity planning: a minimal cost analysis model. J Med Syst 21:309–322
Agarwal S, Joshi A, Finin T, Yesha Y (2007) A pervasive computing system for the operating room of the future. Mob Netw Appl 12:215–228
Doryab A, Togelius J, Bardram J (2012) Activity-aware recommendation for collaborative work in operating rooms. In: Proceedings of the 2012 ACM international conference on intelligent user interfaces, pp 301–304
Dexter F, Willemsen-Dunlap A, Lee J (2007) Operating room managerial decision-making on the day of surgery with and without computer recommendations and status displays. Anesth Analg 105:419–429
Avery DM III, Matullo KS (2013) The efficiency of a dedicated staff on operating room turnover time in hand surgery. J Hand Surg 39:108–110
Radcliff KE, Rasouli MR, Neusner A, Kepler CK, Albert TJ, Rihn JA, Hilibrand AS, Vaccaro AR (2013) Preoperative delay of more than 1 h increases the risk of surgical site infection. Spine 8:1318–1323
Yu J, Smith VA, Wang PP, Hartemink AJ, Jarvis ED (2004) Advances to Bayesian network inference for generating causal networks from observational biological data. Bioinformatics 20(18):3594–3603
Jackson TD, Wannares JJ, Lancaster RT, Rattner DW, Hutter MM (2011) Does speed matter? The impact of operative time on outcome in laparoscopic surgery. Surg Endosc 25(7):2288–2295
Procter L, Davenport D, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg 210(1):60-5.e1-2
Harrop JS, Styliaras JC, Ooi YC, Radcliff KE, Vaccaro AR, Wu C (2012) Contributing factors to surgical site infections. J Am Acad Orthop Surg 20:94–101
Schuster M, Pezzella M, Taube C, Bialas E, Diemer M, Bauer M (2013) Delays in starting morning operating lists: an analysis of more than 20,000 cases in 22 German hospitals. Dtsch Artebl Int 110:237–243
Liu CC, Chang CH, Su MC, Chu HT, Hung SH, Wong JM, Wang PC (2011) RFID-initiated workflow control to facilitate patient safety and utilization efficiency in operation theater. Comput Methods Programs Biomed 3:435–442
Acknowledgments
We acknowledge Linda Moore from Houston Methodist for an interesting discussion on the ACS-NSQIP and potential correlation analysis with our SmartOR data. We also thank the Dunn OR team for their cooperation on the clinical study, and we express our gratitude to Michael Garcia for his interest, support, and feedback on our system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Albert Y. Huang, Guillaume Joerger, Remi Salmon, Vadim Sherman, Brian J. Dunkin, Barbara L. Bass, and Marc Garbey have no disclosures and no conflicts of interest.
Rights and permissions
About this article
Cite this article
Huang, A.Y., Joerger, G., Salmon, R. et al. A robust and non-obtrusive automatic event tracking system for operating room management to improve patient care. Surg Endosc 30, 3638–3645 (2016). https://doi.org/10.1007/s00464-015-4610-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4610-2