Abstract
Introduction
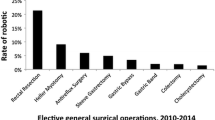
While the penetrance of robotic surgery into field of urology and gynecology has been significant, general surgeons have been slower adopters. We sought to compare laparoscopy and RAS among five different general surgical procedures with various penetrance of MIS.
Methods
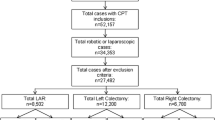
Following IRB approval, the New York Statewide Planning and Research Cooperative System administrative data were used to identify five common laparoscopic general surgery procedures: cholecystectomy, colectomy, esophageal fundoplication (EF), Roux-en-Y gastric bypass (RYGB), and sleeve gastrectomy (SG) between 2008 and 2012. ICD-9 codes were used to select laparoscopic versus robotic procedures. Procedures were compared based on any complication and hospital length of stay (HLOS). Following descriptive analysis, propensity score analysis was used to estimate the population average differences between patients who underwent robotic-assisted and laparoscopic procedures.
Results
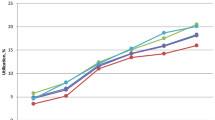
There were 1458 patients who had undergone robotic-assisted surgery and 166,790 patients who had undergone laparoscopic surgery among the five procedures between 2008 and 2012. Of the 1458 robotic cases, 186 were cholecystectomy, 307 were RYGB, 118 were SG, 288 were EF, and 559 were colectomy. Initial univariate analysis showed a significantly higher rate of overall complications and HLOS in the laparoscopic group compared to the robotic-assisted group. Laparoscopic colectomy had a significantly higher rate of complications and longer length of stay compared to robotic approaches. No difference in complications or HLOS was seen in the cholecystectomy group. Following propensity score analysis, patients who had undergone robotic-assisted colectomy had significantly lower rate of complications compared to those who underwent conventional laparoscopic procedure (p value = 0.0022). In addition, patients who underwent robotic-assisted SG had on average 1.22 days longer HLOS (p value = 0.0037).
Conclusion
Robotic approaches may facilitate safer adoption of minimally invasive approaches in areas where penetrance of conventional laparoscopy is low, such as in colorectal surgery.
Similar content being viewed by others
References
Mühe E (1991) Laparoscopic cholecystectomy—late results. Langenbecks Arch Chir Suppl Kongressbd. http://www.ncbi.nlm.nih.gov/pubmed/1838946
Wei HB, Wei B, Qi CL et al (2011) Laparoscopic versus open gastrectomy with D2 lymph node dissection for gastric cancer: a meta-analysis. Surg Laparosc Endosc Percutan Tech 21(6):283–390
Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J (2011) Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg 213(2):261–266
Bliss LA, Yang CJ, Kent TS, Ng SC, Critchlow JF, Tseng JF (2014) Appendicitis in the modern era: universal problem and variable treatment. Surg Endosc 29(7):1897–1902
Csujesz N, Ricciardi R, Tseng JF, Shah SA (2008) Current status of surgical management of acute cholecystitis in the United States. World J Surg 32:2230–2236
Carmichael JS, Masoomi H, Mills S, Stamos MJ, Nguyen MD (2011) Utilization of laparoscopy in colorectal surgery fro cancer at academic medical centers: does site of surgery affect rate of laparoscopy? Am Surg 77(10):1300–1304
Rea JD, Cone MM, Diggs BS, Deveney KE, Lu KC, Herzig DO (2011) Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg 254(2):281–288
Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikoc D (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure. Ann Surg 256(3):462–468
Cirocchi R, Partelli S, Trastulli S et al (2013) A systematic review on robotic pancreaticoduodenectomy. Surg Oncol 22:238–246
Elixhauser A, Syeiner C, Harris D (1998) Co-morbidity measures for use with administrative data. Med Care 36:8–27
Rosenbaum PR, Rubin DB (1983) The central role of propensity score in observational studies for causal effects. Biometrika 70:41–55
Faries DE, Leon AC, Haro JM, Obenchain RL (2010) Analysis of observational health care data using SAS. SAS Institute Inc., Cary, NC
Austin PC, Grootendorst P, Anderson GM (2007) A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 26:734–753
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J 51:171–184
Rosenbaum PR (1995) Observational studies. Springer, New York
Rosenbaum PR (2007) Sensitivity analysis for m-estimates, tests and confidence intervals in matched observational studies. Biometrics 63:456–464
Nguyen NT, Nguyen B, Shih A, Smith B, Hofmann S (2013) Use of laparoscopy in general surgical operations at academic centers. Surg Obes Relat Dis 9:15–20
Villamere J, Gebhard A, Vu S, Nguyen NT (2014) Utilization and outcome of laparoscopic versus robotic general and bariatric surgical procedures at Academic Medical Centers. Surg Endosc 29(7):1729–1736
Acknowledgments
We would like to thank the Foundation for Surgical Fellows for their support of our fellowship program. We also acknowledge the biostatistical consultation and support from the Biostatistical Consulting Core at the School of Medicine, Stony Brook University.
Disclosures
Dr. Pryor has Ownership interest in Transenterics, speaker for Gore and Novadaq, and consults for Freehold Medical and Intuitive. Dr. Telem is a consultant for Ethicon, speaker for Gore, and receives research funding from Cook. Dr. Altieri, Dr. Talamini, Dr. Yang, Dr. Halbert, Ms. Zhu have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Altieri, M.S., Yang, J., Telem, D.A. et al. Robotic approaches may offer benefit in colorectal procedures, more controversial in other areas: a review of 168,248 cases. Surg Endosc 30, 925–933 (2016). https://doi.org/10.1007/s00464-015-4327-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4327-2