Abstract
Background
During peroral esophageal myotomy (POEM) for the treatment of achalasia, the optimal distal gastric myotomy length is unknown. In this study, we used a functional lumen imaging probe (FLIP) to intraoperatively measure the effect of variable distal myotomy lengths on esophagogastric junction (EGJ) distensibility.
Methods
EGJ distensibility index (DI) (minimum cross-sectional area divided by intrabag pressure) was measured with FLIP after each operative step. Each patient’s myotomy was performed in four increments from proximal to distal: (1) an esophageal myotomy (from 6 cm proximal to the EGJ to 1 cm proximal to it), (2) a myotomy ablating the lower esophageal sphincter (LES) complex (from 1 cm proximal to the EGJ to 1 cm distal to it), (3) an initial gastric extension (from 1 cm distal to the EGJ to 2 cm distal), and (4) a final gastric extension (from 2 cm distal to the EGJ to 3 cm distal).
Results
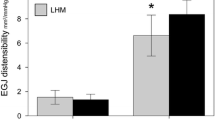
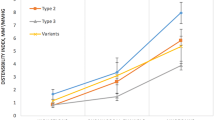
Measurements were taken in 16 achalasia patients during POEM. POEM resulted in an overall increase in DI (pre 1.2 vs. post 7.2 mm2/mmHg, p < .001). Initial creation of the submucosal tunnel resulted in a threefold increase in DI (1.2 vs. 3.6 mm2/mmHg, p < .001). When the myotomy was then performed in a stepwise fashion from proximal to distal, the initial esophageal myotomy component had no effect on DI. Subsequent myotomy extension across the LES complex resulted in an increase in DI, as did the initial gastric myotomy extension (to 2 cm distal to the EGJ). The final gastric myotomy extension (to 3 cm distal) had no further effect.
Conclusions
During POEM, creation of the submucosal tunnel prior to myotomy resulted in a marked improvement in EGJ physiology. Myotomy extension across the LES complex and to 2 cm onto the gastric wall resulted in the normalization of EGJ distensibility, whereas subsequent extension to 3 cm distal to the EGJ did not increase compliance further.

Similar content being viewed by others
References
Triadafilopoulos G, Boeckxstaens GE, Gullo R, Patti MG, Pandolfino JE, Kahrilas PJ, Duranceau A, Jamieson G, Zaninotto G (2012) The Kagoshima consensus on esophageal achalasia. Dis Esophagus 25:337–348
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Teitelbaum EN, Soper NJ, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Hirano I, Hungness ES (2014) Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc 28:3359–3365
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259:1098–1103
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138:490–495 discussion 5–7
Wright AS, Williams CW, Pellegrini CA, Oelschlager BK (2007) Long-term outcomes confirm the superior efficacy of extended Heller myotomy with Toupet fundoplication for achalasia. Surg Endosc 21:713–718
Salvador R, Caruso V, Costantini M, Parise P, Nicoletti L, Cavallin F, Zanatta L, Bardini R, Ancona E, Zaninotto G (2014) Shorter myotomy on the gastric site (≤2.5 cm) provides adequate relief of dysphagia in achalasia patients. Dis Esophagus. doi:10.1111/dote.12226
Pandolfino JE, de Ruigh A, Nicodeme F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil 25:496–501
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143:328–335
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodeme F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29:522–528
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Clouse RE, Staiano A, Alrakawi A, Haroian L (2000) Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol 95:2720–2730
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17:228–235
McMahon BP, Frokjaer JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H (2007) The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol 292:G377–G384
Perretta S, McAnena O, Botha A, Nathanson L, Swanstrom L, Soper NJ, Inoue H, Ponsky J, Jobe B, Marescaux J, Dallemagne B (2013) Acta from the EndoFLIP(R) Symposium. Surg Innov 20:545–552
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodeme F, Lin Z, Hungness ES (2014) An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc 28:2840–2847
Ayazi S, Hagen JA, Zehetner J, Ross O, Wu C, Oezcelik A, Abate E, Sohn HJ, Banki F, Lipham JC, DeMeester SR, Demeester TR (2009) The value of high-resolution manometry in the assessment of the resting characteristics of the lower esophageal sphincter. J Gastrointest Surg 13:2113–2120
Kwiatek MA, Pandolfino JE, Kahrilas PJ (2011) 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil 23:e461–e469
Nicodeme F, Lin Z, Pandolfino JE, Kahrilas PJ (2013) Esophagogastric Junction pressure morphology: comparison between a station pull-through and real-time 3D-HRM representation. Neurogastroenterol Motil 25:e591–e598
Ilczyszyn A, Hamaoui K, Cartwright J, Botha A. (2015) Intraoperative distensibility measurement during laparoscopic Heller’s myotomy for achalasia may reduce the myotomy length without compromising patient outcome. Dis Esophagus. doi:10.1111/dote.12343
Acknowledgments
This work was supported by R01 DK56033 (PJK) and R01 DK092217 (JEP) from the Public Health Service. The authors would like to acknowledge Rowena Martinez, RN, and Colleen Krantz, RN, for their help in coordinating the clinical aspects of this study.
Disclosures
Nathaniel Soper is on the scientific advisory boards of TransEnterix and Miret Surgical, which are unrelated to this study. Eric Hungness receives an honorarium for educational activities from Baxter, which is unrelated to this study. Ezra Teitelbaum, Joel Sternbach, Rym El Khoury, John Pandolfino, Peter Kahrilas, and Zhiyue Lin have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teitelbaum, E.N., Sternbach, J.M., El Khoury, R. et al. The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc 30, 745–750 (2016). https://doi.org/10.1007/s00464-015-4269-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4269-8