Abstract
Background
Peroral endoscopic myotomy (POEM) has been performed as a novel endoscopic procedure to treat achalasia with favorable outcome. The objective of this study was to assess the outcome of POEM in our initial series and to assess the safety and efficacy of POEM in a variety of esophageal motility-related clinical problems.
Methods
This is a retrospective cross-sectional study involving all patients with esophageal motility disorders defined by the Chicago classification, who had undergone consideration for POEM at our institution. Validated questionnaires such as gastroesophageal reflux disease health-related quality of life (GERD-HRQL), reflux symptom index (RSI) and achalasia disease-specific health-related quality of life were obtained pre- and postoperatively.
Results
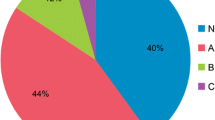
From January 2013 to October 2014, a total of 35 POEMs (achalasia n = 25, non-achalasia n = 10) were performed on 33 patients (female n = 20, male n = 13, mean age 56.9 years). There was no mortality. The rate of inadvertent mucosotomy was 17.1 %. The rate of complications requiring interventions was 5.7 %. During a mean follow-up period of 7 months (range 0.5–17), 92 % of patients with achalasia and 75 % of those with non-achalasia motility disorders had a symptomatic improvement in dysphagia. Chest pain was completely resolved in all patients with achalasia (8/8) and 80 % of patients with non-achalasia (4/5). The GERD-HRQL, RSI and dysphagia scores significantly improved after POEM in patients with achalasia. There was a significant improvement in GERD-HRQL and RSI scores, and a trend toward lower dysphagia score in patients with non-achalasia.
Conclusions
The outcome of POEM to treat achalasia and non-achalasia motility disorders is consistent with previous studies. Potential benefit of POEM includes not only its flexibility to adjust the length and location of myotomy but also the ability to extend myotomy proximally without thoracoscopy or thoracotomy. POEM can be combined with laparoscopic procedures and used as “salvage” for localized esophageal dysmotility.






Similar content being viewed by others
References
Francis DL, Katzka DA (2010) Achalasia: update on the disease and its treatment. Gastroenterology 139(2):369–374
Goldblum JR, Rice TW, Richter JE (1996) Histopathologic features in esophagomyotomy specimens from patients with achalasia. Gastroenterology 111(3):648–654
Goldblum JR, Whyte RI, Orringer MB, Appelman HD (1994) Achalasia. A morphologic study of 42 resected specimens. Am J Surg Pathol 18(4):327–337
Birgisson S, Richter JE (1997) Achalasia: What’s new in diagnosis and treatment? Dig Dis 15(Suppl 1):1–27
Boeckxstaens GE, Annese V, des Varannes SB et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816
Campos GM, Vittinghoff E, Rabl C et al (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249(1):45–57
Bonatti H, Hinder RA, Klocker J et al (2005) Long-term results of laparoscopic Heller myotomy with partial fundoplication for the treatment of achalasia. Am J Surg 190(6):874–878
Costantini M, Zaninotto G, Guirroli E et al (2005) The laparoscopic Heller-Dor operation remains an effective treatment for esophageal achalasia at a minimum 6-year follow-up. Surg Endosc 19(3):345–351
Gockel I, Junginger T, Eckardt VF (2006) Long-term results of conventional myotomy in patients with achalasia: a prospective 20-year analysis. J Gastrointest Surg 10(10):1400–1408
Richards WO, Torquati A, Holzman MD et al (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240(3):405–412 discussion 412–405
Kahrilas PJ, Ghosh SK, Pandolfino JE (2008) Esophageal motility disorders in terms of pressure topography: the Chicago classification. J Clin Gastroenterol 42(5):627–635
Inoue H, Minami H, Kobayashi Y et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271
Stavropoulos SN, Desilets DJ, Fuchs KH et al (2014) Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc 80(1):1–15
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259(6):1098–1103
Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V (2012) Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis 44(10):827–832
Hungness ES, Teitelbaum EN, Santos BF et al (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17(2):228–235
Inoue H, Tianle KM, Ikeda H et al (2011) Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin 21(4):519–525
Sharata AM, Dunst CM, Pescarus R et al (2015) Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 19(1):161–170
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256(4):659–667
von Renteln D, Inoue H, Minami H et al (2012) Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 107(3):411–417
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20(2):130–134
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16(2):274–277
Urbach DR, Tomlinson GA, Harnish JL, Martino R, Diamant NE (2005) A measure of disease-specific health-related quality of life for achalasia. Am J Gastroenterol 100(8):1668–1676
Pasricha PJ, Hawari R, Ahmed I et al (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39(9):761–764
Stavropoulos SN, Modayil RJ, Friedel D, Savides T (2013) The international per oral endoscopic myotomy survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc 27(9):3322–3338
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77(5):719–725
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanstrom LL (2005) Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg 140(9):827–833 discussion 833–824
Rawlings A, Soper NJ, Oelschlager B et al (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 26(1):18–26
Disclosures
Toshitaka Hoppo, Shyam J. Thakkar, Lana Y. Schumacher, Yoshihiro Komatsu, Steve Choe, Amit Shetty, Sara Bloomer, Emily J. Lloyd, Ali H. Zaidi, Mathew A. VanDeusen, Rodney J. Landreneau, Abhijit Kulkarni and Blair A. Jobe have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoppo, T., Thakkar, S.J., Schumacher, L.Y. et al. A utility of peroral endoscopic myotomy (POEM) across the spectrum of esophageal motility disorders. Surg Endosc 30, 233–244 (2016). https://doi.org/10.1007/s00464-015-4193-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4193-y