Abstract
Introduction
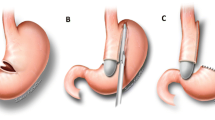
Surgical management of medically refractory gastroparesis remains a challenge. Case series and small retrospective studies describe clinical benefits from surgical intervention; however, no study reports the efficacy of gastric electrical stimulation (GES) or Roux-en-Y gastrojejunostomy with or without near-total gastrectomy (RYGJ) in morbidly obese patients with severe gastroparesis.
Methods
A chart review was performed on all morbidly obese patients (BMI > 35 kg/m2) who underwent GES or RYGJ for medically refractory gastroparesis from March 2002 to December 2012 at the Cleveland Clinic. The main outcomes examined were symptom improvement, postoperative complications, and change in BMI.
Results
A total of 20 morbidly obese patients underwent GES placement. Seven morbidly obese patients had RYGJ with or without resection of the remnant stomach surgery. All operations were completed laparoscopically. In GES group, 18 patients had initial symptom improvement (90 %) and 11 (55 %) rated their symptom improved at the last follow-up. During the average 23 months’ follow-up, 9 patients (45 %) experienced at least one readmission for gastrointestinal reasons. Early complications included two infections at a simultaneously placed J-tube site and one seroma. In the RYGJ group, all patients, including 4 patients who failed GES and subsequently converted to RYGJ, experienced short-term symptom improvement and 5 patients (71 %) rated their symptoms as improved at last follow-up. One duodenal stump leak happened in the RYGJ group. There were no 30-day mortalities in either group. The BMI change after GES implantation was 0.6 ± 4 kg/m2 versus −7.7 ± 4 kg/m2 after RYGJ (p < 0.01).
Conclusion
GES implantation and RYGJ are both effective in terms of symptom control for medically refractory gastroparesis in morbidly obese. Both options can be performed in a minimally invasive fashion with low morbidity. Patients who have no improvement of symptoms for refractory gastroparesis after GES implantation can be successfully converted laparoscopically to RYGJ.
Similar content being viewed by others
References
Abell T, Lou J et al (2003) Gastric electrical stimulation for gastroparesis improves nutritional parameters at short, intermediate, and long-term follow-up. JPEN 27(4):277–281
Abell T, McCallum R et al (2003) Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology 125(2):421–428
Abell TL, Bernstein RK et al (2006) Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil 18(4):263–283
Abell TL, Van Cutsem E et al (2002) Gastric electrical stimulation in intractable symptomatic gastroparesis. Digestion 66(4):204–212
Arts J, Holvoet L et al (2007) Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther 26(9):1251–1258
Boaz M, Kislov J et al (2011) Obesity and symptoms suggestive of gastroparesis in patients with type 2 diabetes and neuropathy. J Diabetes Complicat 25(5):325–328
Borrazzo EC (2013) Surgical management of gastroparesis: gastrostomy/jejunostomy tubes, gastrectomy, pyloroplasty, gastric electrical stimulation. J Gastrointest Surg 17(9):1559–1561
Camilleri M, Parkman HP et al (2013) Clinical guideline: management of gastroparesis. Am J Gastroenterol 108(1):18–37 quiz 38
Chen JD, Xu X et al (2005) Efficiency and efficacy of multi-channel gastric electrical stimulation. Neurogastroenterol Motil 17(6):878–882
De Block CE, De Leeuw IH et al (2005) Impact of overweight on chronic microvascular complications in type 1 diabetic patients. Diabetes Care 28(7):1649–1655
Forstner-Barthell AW, Murr MM et al (1999) Near-total completion gastrectomy for severe postvagotomy gastric stasis: analysis of early and long-term results in 62 patients. J Gastrointest Surg 3(1):15–21 discussion 21-13
Friedenberg FK, Parkman HP (2008) Persistent nausea and abdominal pain in a patient with delayed gastric emptying. Clin Gastroenterol Hepatol 6(12):1309–1314
Hasler WL (2007) Gastroparesis: symptoms, evaluation, and treatment. Gastroenterol Clin North Am 36(3):619–647 ix
Hasler WL (2011) Gastroparesis: pathogenesis, diagnosis and management. Nat Rev Gastroenterol Hepatol 8(8):438–453
Hasler WL, Wilson LA et al (2011) Bloating in gastroparesis: severity, impact, and associated factors. Am J Gastroenterol 106(8):1492–1502
Jones MP, Maganti K (2003) A systematic review of surgical therapy for gastroparesis. Am J Gastroenterol 98(10):2122–2129
Jung HK, Choung RS et al (2009) The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology 136(4):1225–1233
Keller DS, Parkman HP et al (2013) Surgical outcomes after gastric electric stimulator placement for refractory gastroparesis. J Gastrointest Surg 17(4):620–626
Kibirige M, Metcalf B et al (2003) Testing the accelerator hypothesis: the relationship between body mass and age at diagnosis of type 1 diabetes. Diabetes Care 26(10):2865–2870
Lacy BE, Crowell MD et al (2004) The treatment of diabetic gastroparesis with botulinum toxin injection of the pylorus. Diabetes Care 27(10):2341–2347
Libman IM, Pietropaolo M et al (2003) Changing prevalence of overweight children and adolescents at onset of insulin-treated diabetes. Diabetes Care 26(10):2871–2875
Nguyen LB, Parker S, Snape WJ (2007) Is pyloroplasty a surgical option in the treatment of refractory gastroparesis? Gastroenterology 132:M1151
Ma J, Rayner CK et al (2009) Diabetic gastroparesis: diagnosis and management. Drugs 69(8):971–986
Maranki JL, Lytes V et al (2008) Predictive factors for clinical improvement with Enterra gastric electric stimulation treatment for refractory gastroparesis. Dig Dis Sci 53(8):2072–2078
Mason RJ, Lipham J et al (2005) Gastric electrical stimulation: an alternative surgical therapy for patients with gastroparesis. Arch Surg 140(9):841–846 discussion 847-848
McCallum RW, Lin Z et al (2011) Gastric electrical stimulation improves outcomes of patients with gastroparesis for up to 10 years. Clin Gastroenterol Hepatol 9(4):314–319 e311
McCallum RW, Snape W et al (2010) Gastric electrical stimulation with Enterra therapy improves symptoms from diabetic gastroparesis in a prospective study. Clin Gastroenterol Hepatol 8(11):947–954 quiz e116
Miller LS, Szych GA et al (2002) Treatment of idiopathic gastroparesis with injection of botulinum toxin into the pyloric sphincter muscle. Am J Gastroenterol 97(7):1653–1660
Parkman HP, Yates K et al (2011) Clinical features of idiopathic gastroparesis vary with sex, body mass, symptom onset, delay in gastric emptying, and gastroparesis severity. Gastroenterology 140(1):101–115
Smyth S, Heron A (2006) Diabetes and obesity: the twin epidemics. Nat Med 12(1):75–80
Soykan I, Sivri B et al (1998) Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci 43(11):2398–2404
Speicher JE, Thirlby RC et al (2009) Results of completion gastrectomies in 44 patients with postsurgical gastric atony. J Gastrointest Surg 13(5):874–880
Tapia J, Murquia R (1999) Jejunostomy: techniques, indications, and complication. World J Surg 23(6):596–602
Timratana P, El-Hayek K et al (2013) Laparoscopic gastric electrical stimulation for medically refractory diabetic and idiopathic gastroparesis. J Gastrointest Surg 17(3):461–470
Wang YR, Fisher RS et al (2008) Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995–2004. Am J Gastroenterol 103(2):313–322
Watkins PJ, Buxton-Thomas MS et al (2003) Long-term outcome after gastrectomy for intractable diabetic gastroparesis. Diabet Med 20(1):58–63
Zehetner J, Ravari F et al (2013) Minimally invasive surgical approach for the treatment of gastroparesis. Surg Endosc 27(1):61–66
Disclosures
Zhuo Sun, John Rodriguez, John McMichael, Bipan Chand, Deanne Nash, Stacy Brethauer, Phillip Schauer, Kevin El-Hayek, and Matthew Kroh have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, Z., Rodriguez, J., McMichael, J. et al. Surgical treatment of medically refractory gastroparesis in the morbidly obese. Surg Endosc 29, 2683–2689 (2015). https://doi.org/10.1007/s00464-014-3990-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3990-z