Abstract
Background
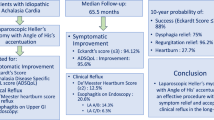
The type of anti-reflux procedure to be used as an adjunct to laparoscopic Heller’s cardiomyotomy (LHCM) in Achalasia cardia is controversial. We compared Angle of His accentuation and Dor fundoplication in a randomized controlled trial.
Methods
From May 2010 to October 2013, 62 patients undergoing LHCM were randomized to receive either Dor fundoplication (Dor group) or Angle of His accentuation (AOH group) as an anti-reflux procedure. Symptomatic outcome was evaluated using modified Mellow and Pinkas scale for dysphagia and modified DeMeester’s score for regurgitation and heartburn. Achalasia-specific quality-of-life (QOL) questionnaire was used to assess quality of life. The primary outcome was symptomatic relief and the secondary outcome was postoperative heartburn. Statistical analysis was done using SPSS software.
Results
All the procedures were completed laparoscopically with no mortality. Morbidity was similar in the two groups (6.4 %). Median operative time was higher in Dor group (170 vs 130 min). At a median follow-up of 21 months relief of dysphagia, regurgitation, and heartburn was seen in 87, 90.3, and 90.3 % patients in Dor group versus 93.5, 96.7, and 77.4 % in AOH group patients with significant improvement in symptom scores. Improvement was similar in both groups with no statistically significant difference in the symptom scores (p = 0.48 for dysphagia, p = 0.37 for regurgitation, and p = 0.19 for heartburn). The QOL improved in both groups [62.3 to 12.3 (p = 0.02) in Dor group and 63.9–13 (p = 0.02) in AOH group] with no statistically significant difference between the two groups (p = 0.96). There was no statistically significant difference in the postoperative heartburn between the two groups (p = 0.19).
Conclusion
Laparoscopic Heller's cardiomyotomy with either Angle of His accentuation or Dor fundoplication leads to similar improvement in symptoms and quality of life.

Similar content being viewed by others
References
Fernández AF, Martínez MA, Ruiz J, Torres R, Faife B, Torres JR (2003) Six years of experience in laparoscopic surgery of esophageal achalasia. Surg Endosc 17(1):153–156
Eckardt VF, Gockel I, Bernhard G (2004) Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 53:629–633
Patti MG, Fisichella PM, Perretta S, Galvani C, Gorodner MV, Robinson T (2003) Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196(5):698–703
Ghoshal UC, Chaudhuri S, Pal BB, Dhar K, Ray G, Banerjee PK (2001) Randomized controlled trial of intrasphincteric botulinum toxin A injection versus balloon dilatation in treatment of achalasia cardia. Dis Esophagus 14(3–4):227–231
Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD (2010) Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 24(11):2647–2669
Parshad R, Hazrah P, Saraya A, Garg P, Makharia G (2008) Symptomatic outcome of laparoscopic cardiomyotomy without an antireflux procedure: experience in initial 40 cases. Surg Laparosc Endosc Percutan Tech 18(2):139–143
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R et al (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240(3):405–412
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F et al (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249(1):45–57
Falkenback D, Johansson J, Oberg S, Kjellin A, Wenner J, Zilling T et al (2003) Heller’s esophagomyotomy with or without a 360 degrees floppy Nissen fundoplication for achalasia. Long-term results from a prospective randomized study. Dis Esophagus 16(4):284–290
Patti MG, Herbella FA (2010) Fundoplication after laparoscopic Heller myotomy for esophageal achalasia: what type? J Gastrointest Surg 14(9):1453–1458
Wei M-T, He Y-Z, Deng X-B, Zhang Y-C, Yang T-H, Jin C-W, Hu B, Wang Z-Q (2013) Is Dor fundoplication optimum after laparoscopic Heller myotomy for achalasia? A meta-analysis. World J Gastroenterol 19(43):7804–7812
Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, Russo G, Izzo D, Russo F, Pizza F, Del Genio G, Del Genio A (2005) A total fundoplication is not an obstacle to esophageal emptying after Heller myotomy for achalasia: results of a long term follow-up. Ann Surg 241:614–621
Rebecchi F, Giaccone C, Farinella E, Campaci R, Morino M (2008) Randomized controlled trial of laparoscopic Heller myotomy plus Dor fundoplication versus Nissen fundoplication for achalasia: long-term results. Ann Surg 248(6):1023–1030
Rawlings A, Soper NJ, Oelschlager B, Swanstrom L, Matthews BD, Pellegrini C et al (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 26:18–26
Smith CD, Stival A, Howell DL, Swafford V (2006) Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than heller myotomy alone. Ann Surg 243(5):579–584
Ramacciato G, D’Angelo FA, Aurello P, Del Gaudio M, Varotti G, Mercantini P et al (2005) Laparoscopic Heller myotomy with or without partial fundoplication: a matter of debate. World J Gastroenterol 11(10):1558–1561
Mellow MH, Pinkas H (1985) Endoscopic laser therapy for malignancies affecting the esophagus and gastroesophageal junction. Analysis of technical and functional efficacy. Arch Intern Med 145(8):1443–1446
Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB (1976) Patterns of gastroesophageal reflux in health and disease. Ann Surg 184(4):459–470
Urbach DR, Tomlinson TA, Harnish JL et al (2005) A measure of disease-specific health-related quality of life for achalasia. Am J Gastroenterol 100:1668–1676
Shiino Y, Filipi CJ, Awad ZT, Tomonaga T, Marsh RE (1999) Surgery for achalasia. J Gastrointest Surg 3(5):447–455
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A et al (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230(4):587–593
Lyass S, Thoman D, Steiner JP, Phillips E (2003) Current status of an antireflux procedure in laparoscopic Heller myotomy. Surg Endosc 17(4):554–558
Bloomston M, Rosemurgy AS (2002) Selective application of fundoplication during laparoscopic heller myotomy ensures favorable outcomes. Surg Laparosc Endosc Percutan Tech 12(5):309–315
Kurian AA, Bhayani N, Sharata A, Reavis K, Dunst CM, Swanstro¨m LL (2013) Partial anterior vs partial posterior fundoplication following transabdominal esophagocardiomyotomy for achalasia of the esophagus. JAMA Surg 148(1):85–90
Patti MG, Molena D, Fisichella PM, Whang K, Yamada H, Perretta S et al (2001) Laparoscopic Heller myotomy and Dor fundoplication for achalasia: analysis of successes and failures. Arch Surg 136(8):870–877
Perrone JM, Frisella MM, Desai KM, Soper NJ (2004) Results of laparoscopic Heller–Toupet operation for achalasia. Surg Endosc 18(11):1565–1571
Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A et al (2002) Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg 235(2):186–192
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138(5):490–495
Panchanatheeswaran K, Parshad R, Rohila J, Saraya A, Makharia GK, Sharma R (2013) Laparoscopic Heller’s cardiomyotomy: a viable treatment option for sigmoid oesophagus. Interact CardioVasc Thorac Surg 16:49–54
Patti MG, Feo CV, Arcerito M, De Pinto M, Tamburini A, Diener U et al (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 44(11):2270–2276
Gholoum S, Feldman LS, Andrew CG, Bergman S, Demyttenaere S, Mayrand S, Stanbridge DD, Fried GM (2006) Relationship between subjective and objective outcome measures after Heller myotomy and Dor fundoplication for achalasia. Surg Endosc 20(2):214–219
Johnston PW, Johnston BT, Collins BJ, Collins JS, Love AH (1993) Audit of the role of oesophageal manometry in clinical practice. Gut 34(9):1158–1161
Meshkinpour H, Glick ME, Sanchez P, Tarvin J (1982) Esophageal manometry: a benefit and cost analysis. Dig Dis Sci 27(9):772–775
Disclosures
Dr. Pavithra Balakrishna, Dr. Rajinder Parshad, Dr. Jitender Rohila, Dr. Anoop Saraya, Dr. Govind Makharia and Dr. Raju Sharma individually have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balakrishna, P., Parshad, R., Rohila, J. et al. Symptomatic outcome following laparoscopic Heller’s cardiomyotomy with Dor fundoplication versus laparoscopic Heller’s cardiomyotomy with angle of His accentuation: results of a randomized controlled trial. Surg Endosc 29, 2344–2351 (2015). https://doi.org/10.1007/s00464-014-3958-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3958-z