Abstract
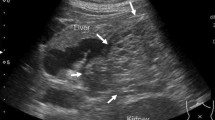
Laparoscopic vascular repair is technically challenging in pancreatic surgeries. We present a case of a 42-year-old woman who was initially admitted to our hospital because of upper abdominal pain. Preoperative abdominal enhanced CT scan revealed a cystic mass near the spleen that was 4.7 × 4.3 × 3 (cm) in dimension. Therefore, we performed laparoscopic spleen-preserving distal pancreatectomy. In this procedure, we repaired spleen-related vessels with laparoscopic suture due to the adhesion between the vessels and the tumor. Finally, the spleen was preserved with good blood supply. This procedure took 200 min and the estimated blood loss was 360 ml. The postoperative abdominal Doppler ultrasound carried out 6 days after surgery indicated blood supply to the spleen was good and there was no thrombosis. The patient was discharged without any complications on postoperative day 7. The pathological diagnosis was pancreatic mucinous cystadenoma.
Article PDF
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Disclosures
Xin Wang, Yongbin Li, and Bing Peng have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MPG 274002 kb)
Rights and permissions
About this article
Cite this article
Wang, X., Li, Y. & Peng, B. Laparoscopic spleen-preserving distal pancreatectomy with intraoperative vascular repair. Surg Endosc 28, 1330 (2014). https://doi.org/10.1007/s00464-013-3328-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3328-2