Abstract
Background
Readmissions to the hospital within 30 days of discharge (30-day readmission rate) may impact stent use in palliative treatment of cancer.
Objective
Our objective was to investigate the incidence of readmission and factors predicting readmissions and long-term outcomes in patients with self-expanding metal stents (SEMS) placed for malignant obstruction.
Methods
Retrospective analysis of all patients who underwent placement of SEMS from 2007 to 2012 for malignant esophageal, gastroduodenal, and colonic obstruction. Incidence and variables associated with 30-day readmission and long-term outcomes were determined.
Results
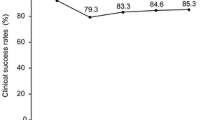
A total of 191 patients underwent stent placement. The 30-day readmission rate was 17.3 % (N = 33). Readmissions were for stent-related complications in 7.3 % (N = 14) and non-stent-related complications in 9.9 % (N = 19). Stent placement was technically successful in 185 of 191 (96.9 %) and clinically successful in 170 of 191 (89.0 %) patients. On long-term follow-up, 32 (16.8 %) patients needed re-intervention. The mean stent patency was 142 days. Readmission within 30 days was independently associated with development of early complications (<7 days) following stent placement (odds ratio [OR] 5.90; 95 % confidence interval [CI] 2.04–17.1), while the stent location did not impact readmission risk. On Cox regression analysis, American Society of Anesthesiologists physical classification (OR 1.36; 95 % CI 1.02–1.87) and stent location in the esophagus (OR 1.82; 95 % CI 1.10–3.02) were independently associated with long-term mortality.
Conclusions
Early complications following stent placement increase the risk of 30-day readmission. SEMS is efficacious long-term for palliation of malignant gastrointestinal obstruction.



Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CI:
-
Confidence interval
- CCI:
-
Charlson comorbidity index
- LOS:
-
Length of hospital stay
- OR:
-
Odds ratio
- SEMS:
-
Self expanding metal stents
References
Ashton C, Kuykendall D, Johnson M et al (1995) The association between the quality of inpatient care and early readmission. Ann Intern Med 122:415–421
Balla U, Malnick S, Schattner A (2008) Early readmissions to the department of medicine as a screening tool for monitoring quality of care problems. Medicine 87:294–300
Benbassat J, Taragin M (2000) Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med 160:1074–1081
Straube B, Blum JD (2009) The policy on paying for treating hospital-acquired conditions: CMS officials respond. Health Aff (Millwood) 28(5):1494–1497
Dormann A, Meisner S, Verin N, Wenk LA (2004) Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy 36:543–550
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99:2051–2057
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246:24–30
Keranen I, Udd M, Lepisto A, Halttunen J, Kylanpaa L (2010) Outcome for self-expandable metal stents in malignant gastroduodenal obstruction: single-center experience with 104 patients. Surg Endosc 24:891–896
Vemulapalli R, Lara LF, Sreenarasimhaiah J, Harford WV, Siddiqui AA (2010) A comparison of palliative stenting or emergent surgery for obstructing incurable colon cancer. Dig Dis Sci 55:1732–1737
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71:560–572
Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW et al (2007) Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc 21:225–233
Larssen L, Medhus AW, Körner H, Glomsaker T, Søberg T, Gleditsch D, Hovde Ø, Tholfsen JK, Skreden K, Nesbakken A, Hauge T (2012) Long-term outcome of palliative treatment with self-expanding metal stents for malignant obstructions of the GI tract. Scand J Gastroenterol 47(12):1504–1505
Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T et al (2004) Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Results of a study and cost-effectiveness analysis. Surg Endosc 18:421–426
van Hooft JE, Fockens P, Marinelli AW, Dutch Colorectal Stent Group et al (2008) Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy 40:184–191
Camunez F, Echenagusia A, Simo G et al (2000) Malignant colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation. Radiology 216:492–497
Schembre DB (2010) Recent advances in the use of stents for esophageal disease. Gastrointest Endosc Clin N Am 20:103–121
Acknowledgments
The study was supported by a research grant from the Inflammatory Bowel Disease Working Group and American College of Gastroenterology Grant (both to U.N.).
Disclosures
Udayakumar Navaneethan, Sudhir Duvuru, Ramprasad Jegadeesan, Preethi G. K. Venkatesh, Norma G. Gutierrez, Jeffrey Hammel, Ravi P. Kiran, and Madhusudhan R. Sanaka have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Navaneethan, U., Duvuru, S., Jegadeesan, R. et al. Factors associated with 30-day readmission and long-term efficacy of enteral stent placement for malignancy. Surg Endosc 28, 1194–1201 (2014). https://doi.org/10.1007/s00464-013-3308-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3308-6