Abstract
Background
This study was designed to evaluate the outcome of laparoscopic cholecystectomy by comparing a new technique using occult-scar incision for laparoscopic cholecystectomy (OSLC) with classic three-port laparoscopic cholecystectomy (CLC). In the occult-scar incision, we moved the subcostal and subxiphoid trocar insertion sites to the suprapubic area so that operative scars were hidden in the pubic hairs and below umbilicus.
Methods
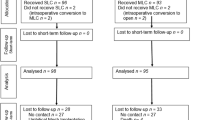
Between July 2009 and 2012, patients undergoing laparoscopic cholecystectomy were randomized to the OSLC or CLC approach after obtaining informed consent. Outcome was measured by operative time, operative complications, hospital length of stay, cost, analgesia required after surgery, and cosmetic outcomes. The patient satisfaction score (PSS) and visual analog score (VAS) also were used to evaluated the level of cosmetic result and postoperative pain.
Results
A total of 75 patients were randomized into CLC (n = 35) and OSLC (n = 40) groups. No patient was converted to an open procedure in either the CLC or OSLC group. No operative complications were reported within 30 days in either group. The PSS of 7 and 30 days after surgery were both significantly higher in the OSLC group than in the CLC group (5.8 ± 1.5 vs. 8.0 ± 1.1, P = 0.03; 6.5 ± 1.2 vs. 9.2 ± 0.8, P = 0.02). The VAS for pain was significantly lower in the OSLC group on postoperative day 3 compared with the CLC group (2.6 ± 1.2 vs. 6.3 ± 0.9, P = 0.01). There was no significant difference in operative time, hospital stay, and cost between the two groups.
Conclusions
The OSLC is a safe and feasible alternative compared with CLC in experienced hands, and it is superior for outcomes regarding pain control and cosmesis.


Similar content being viewed by others
References
Litwin DE, Cahan MA (2008) Laparoscopic cholecystectomy. Surg Clin North Am 88(6):1295–1313
Leggett PL, Churchman-Winn R, Miller G (2000) Minimizing ports to improve laparoscopic cholecystectomy. Surg Endosc 14(1):32–36
Thakur V, Schlachta CM, Jayaraman S (2011) Minilaparoscopic versus conventional laparoscopic cholecystectomy: a systematic review and meta-analysis. Ann Surg 253(2):244–258
Auyang ED, Santos BF, Enter DH et al (2011) Natural orifice translumenal endoscopic surgery (NOTES(R)): a technical review. Surg Endosc 25(10):3135–3148
Wong JS, Cheung YS, Fong KW et al (2012) Comparison of postoperative pain between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: prospective case-control study. Surg Laparosc Endosc Percutan Tech 22(1):25–28
Garg P, Thakur JD, Singh I et al (2012) A prospective controlled trial comparing single-incision and conventional laparoscopic cholecystectomy: caution before damage control. Surg Laparosc Endosc Percutan Tech 22(3):220–225
Soper NJ, Stockmann PT, Dunnegan DL et al (1992) Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg 127(8):917–921
Tenconi SM, Boni L, Colombo EM et al (2008) Laparoscopic cholecystectomy as day-surgery procedure: current indications and patients’ selection. Int J Surg 6:S86–S88
Lehmann KS, Ritz JP, Wibmer A et al (2010) The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg 252(2):263–270
Lee PC, Lo C, Lai PS et al (2010) Randomized clinical trial of single incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg 97(7):1007–1012
Roy P, De A (2010) Transumbilical multiple-port laparoscopic cholecystectomy (TUMP-LC): a prospective analysis of 50 initial patients. J Laparoendosc Adv Surg Tech A 20(3):211–217
Fronza JS, Linn JG, Nagle AP et al (2010) A single institution’s experience with single incision cholecystectomy compared to standard laparoscopic cholecystectomy. Surgery 148(4):731–734; discussion 734–736
Hao LX, Liu MY, Zhu HY et al (2012) Single-incision versus conventional laparoscopic cholecystectomy in patients with uncomplicated gallbladder disease: a meta-analysis. Surg Laparosc Endosc Percutan Tech 22(6):487–497
Disclosures
Drs. Lei Zhang, Bijay Sah, Jing Ma, Changzhen Shang, Zejian Huang, and Yajin Chen have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, L., Sah, B., Ma, J. et al. A prospective, randomized, controlled, trial comparing occult-scar incision laparoscopic cholecystectomy and classic three-port laparoscopic cholecystectomy. Surg Endosc 28, 1131–1135 (2014). https://doi.org/10.1007/s00464-013-3289-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3289-5