Abstract
Background
Gastroesophageal reflux disease (GERD) remains a significant problem for the medical community. Many endoluminal treatments for GERD have been developed with little success. Currently, transoral incisionless fundoplication (TIF) attempts to recreate a surgical fundoplication through placement of full-thickness polypropylene H-fasteners. This, the most recent procedure to gain FDA approval, has shown some promise in the early data. However, questions of its safety profile, efficacy, and durability remain.
Methods
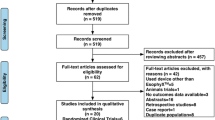
The Cochrane Library and MEDLINE through PubMed were searched to identify published studies reporting on subjective and objective GERD indices after TIF. The search was limited to human studies published in English from 2006 up to March 2012. Data collected included GERD-HRQL and RSI scores, PPI discontinuation and patient satisfaction rates, pH study metrics, complications, and treatment failures. Statistical analysis was performed with weighted t tests.
Results
Titles and abstracts of 214 papers were initially reviewed. Fifteen studies were found to be eligible, reporting on over 550 procedures. Both GERD-HRQL scores (21.9 vs. 5.9, p < 0.0001) and RSI scores (24.5 vs. 5.4, p ≤ 0.0001) were significantly reduced after TIF. Overall patient satisfaction was 72 %. The overall rate of PPI discontinuation was 67 % across all studies, with a mean follow-up of 8.3 months. pH metrics were not consistently normalized. The major complication rate was 3.2 % and the failure rate was 7.2 % across all studies.
Conclusion
TIF appears to provide symptomatic relief with reasonable levels of patient satisfaction at short-term follow-up. A well-designed prospective clinical trial is needed to assess the effectiveness and durability of TIF as well as to identify the patient population that will benefit from this procedure.



Similar content being viewed by others
References
American Gastroenterological Association (2001) The Burden of gastrointestinal diseases. AGA, Bethesda, pp 18–21
Moayyedi P, Leontiadis GI (2012) The risks of PPI therapy. Nat Rev Gastroenterol Hepatol 9:132–139
Linsky A, Gupta K, Lawler EV et al (2010) Proton pump inhibitors and risk for recurrent Clostridium difficile infection. Arch Intern Med 170:772–778
Howell MD, Novack V, Grgurich P et al (2010) Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med 170:784–790
Spechler SJ (1992) Comparison of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med 326:786–792
Finks JF, Wei Y, Birkmeyer JD (2006) The rise and fall of antireflux surgery in the United States. Surg Endosc 20:1698–1701
Barnes WE, Hoddinott KM, Mundy S et al (2011) Transoral incisionless fundoplication offers high patient satisfaction and relief of therapy-resistant typical and atypical symptoms of GERD in community practice. Surg Innov 18:119–129
Bell RC, Freeman KD (2011) Clinical and pH-metric outcomes of transoral esophagogastric fundoplication for the treatment of gastroesophageal reflux disease. Surg Endosc 25:1975–1984
Cadiere GB, Buset M, Muls V et al (2008) Antireflux transoral incisionless fundoplication using EsophyX: 12-month results of a prospective multicenter study. World J Surg 32:1676–1688
Cadiere GB, Van Sante N, Graves JE et al (2009) Two-year results of a feasibility study on antireflux transoral incisionless fundoplication using EsophyX. Surg Endosc 23:957–964
Demyttenaere SV, Bergman S, Pham T et al (2010) Transoral incisionless fundoplication for gastroesophageal reflux disease in an unselected patient population. Surg Endosc 24:854–858
Frazzoni M, Conigliaro R, Manta R et al (2011) Reflux parameters as modified by EsophyX or laparoscopic fundoplication in refractory GERD. Aliment Pharmacol Ther 34:67–75
Hoppo T, Immanuel A, Schuchert M et al (2010) Transoral incisionless fundoplication 2.0 procedure using EsophyX for gastroesophageal reflux disease. J Gastrointest Surg 14:1895–1901
Ihde GM, Besancon K, Deljkich E (2011) Short-term safety and symptomatic outcomes of transoral incisionless fundoplication with or without hiatal hernia repair in patients with chronic gastroesophageal reflux disease. Am J Surg 202:740–746 discussion 746–747
Narsule CK, Burch MA, Ebright MI et al (2012) Endoscopic fundoplication for the treatment of gastroesophageal reflux disease: initial experience. J Thorac Cardiovasc Surg 143:228–234
Nguyen A, Vo T, Nguyen XM et al (2011) Transoral incisionless fundoplication: initial experience in patients referred to an integrated academic institution. Am Surg 77:1386–1389
Petersen RP, Filippa L, Wassenaar EB et al (2012) Comprehensive evaluation of endoscopic fundoplication using the EsophyX™ device. Surg Endosc 26(4):1021–1027
Repici A, Fumagalli U, Malesci A et al (2010) Endoluminal fundoplication (ELF) for GERD using EsophyX: a 12-month follow-up in a single-center experience. J Gastrointest Surg 14:1–6
Testoni PA, Vailati C, Testoni S et al (2012) Transoral incisionless fundoplication (TIF 2.0) with EsophyX for gastroesophageal reflux disease: long-term results and findings affecting outcome. Surg Endosc 26(5):1425–1435
Trad KS, Turgeon DG, Deljkich E (2012) Long-term outcomes after transoral incisionless fundoplication in patients with GERD and LPR symptoms. Surg Endosc 26:650–660
Velanovich V (2010) Endoscopic, endoluminal fundoplication for gastroesophageal reflux disease: initial experience and lessons learned. Surgery 148:646–651 discussion 651-643
Hunter J, Trus T, Branum G et al (1996) A physiologic approach to laparoscopic fundoplication for gastroesophageal reflux disease. Ann Surg 223:673–685
Testoni PA, Corsetti M, Di Pietro S et al (2010) Effect of transoral incisionless fundoplication on symptoms, PPI use, and pH-impedance refluxes of GERD patients. World J Surg 34:750–757
Khajanchee YS, Ujiki M, Dunst CM et al (2009) Patient factors predictive of 24-h pH normalization following endoluminal gastroplication for GERD. Surg Endosc 23:2525–2530
Bergman S, Mikami DJ, Hazey JW et al (2008) Endolumenal fundoplication with EsophyX: the initial North American experience. Surg Innov 15:166–170
Rantanen TK, Salo JA, Sipponen JT (1999) Fatal and life-threatening complications in antireflux surgery: analysis of 5,502 operations. Br J Surg 86:1573–1577
Bell RC, Cadiere GB (2011) Transoral rotational esophagogastric fundoplication: technical, anatomical, and safety considerations. Surg Endosc 25:2387–2399
Disclosures
Mark Wendling, W. Scott Melvin, and Kyle Perry have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wendling, M.R., Melvin, W.S. & Perry, K.A. Impact of transoral incisionless fundoplication (TIF) on subjective and objective GERD indices: a systematic review of the published literature. Surg Endosc 27, 3754–3761 (2013). https://doi.org/10.1007/s00464-013-2961-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2961-0