Abstract
Background
Persistent pain is common after inguinal hernia repair. The methods of surgery and anesthesia influence the risk. Local anesthesia and laparoscopic procedures reduce the risk for postoperative pain in different time perspectives. The aim of this study was to compare open Lichtenstein repair under local anesthesia (LLA) with laparoscopic total extraperitoneal repair (TEP) with respect to postoperative pain.
Methods
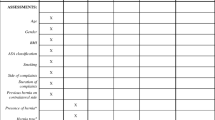
Between 2006 and 2010, a total of 389 men with a unilateral primary groin hernia were randomized, in an open-label study, to either TEP (n = 194) or LLA (n = 195). One patient in the TEP group and four in the LLA group were excluded due to protocol violation. Details about the procedure and patient and hernia characteristics were registered. Patients completed the Inguinal Pain Questionnaire (IPQ) 6 weeks after surgery. [The study is registered in ClinicalTrials.gov (No. NCT01020058)].
Results
A total of 378 (98.4 %) patients completed the IPQ. One hundred forty-eight patients (39.1 %) reported some degree of pain, 22 of whom had pain that affected concentration during daily activities. Men in the TEP group had less risk for pain affecting daily activities (6/191 vs. 16/187; odds ratio [OR] 0.35; 95 % CI 0.13–0.91; p = 0.025). Pain prevented participation in sporting activities less frequently after TEP (4.2 vs. 15.5 %; OR 0.24; 95 % CI 0.09–0.56; p < 0.001). Twenty-nine patients (7.7 %) reported sick leave exceeding 1 week due to groin pain, with no difference between the treatment groups.
Conclusions
Patients who underwent the laparoscopic TEP procedure suffered less pain 6 weeks after inguinal hernia repair than those who underwent LLA. Groin pain affected the LLA patients’ ability to perform strenuous activities such as sports more than TEP patients.


Similar content being viewed by others
References
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev (4):CD002197
van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J (2007) Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 94:506–510
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94:562–565
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336:1541–1547
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD001785
Schmedt CG, Sauerland S, Bittner R (2004) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199
Bittner R, Sauerland S, Schmedt CG (2005) Comparison of endoscopic techniques vs Shouldice and other open nonmesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:605–615
Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Osterberg J, Montgomery A (2006) Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg 93:1060–1068
Grant AM, Scott NW, O’Dwyer PJ (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
MRC Laparoscopic Groin Hernia Trial Group (1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. The MRC Laparoscopic Groin Hernia Trial Group. Lancet 354:185–190
Eklund A, Carlsson P, Rosenblad A, Montgomery A, Bergkvist L, Rudberg C (2010) Long-term cost-minimization analysis comparing laparoscopic with open (Lichtenstein) inguinal hernia repair. Br J Surg 97:765–771
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant AM (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD004703
Jensen P, Mikkelsen T, Kehlet H (2002) Postherniorrhaphy urinary retention-effect of local, regional, and general anesthesia: a review. Reg Anesth Pain Med 27:612–617
Nordin P, Zetterstrom H, Gunnarsson U, Nilsson E (2003) Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. Lancet 362:853–858
Nordin P, Zetterstrom H, Carlsson P, Nilsson E (2007) Cost-effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. Br J Surg 94:500–505
van Veen RN, Mahabier C, Dawson I, Hop WC, Kok NF, Lange JF, Jeekel J (2008) Spinal or local anesthesia in Lichtenstein hernia repair: a randomized controlled trial. Ann Surg 247:428–433
Amid PK, Shulman AG, Lichtenstein IL (1995) The Lichtenstein open “tension-free” mesh repair of inguinal hernias. Surg Today 25:619–625
Amid PK, Shulman AG, Lichtenstein IL (1994) Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg 220:735–737
Nilsson E, Haapaniemi S (1998) Hernia registers and specialization. Surg Clin North Am 78:1141–1155 ix
Swedish Hernia Register T (2010) Annual report 2010. Available at http://www.svensktbrackregister.se. Accessed 05 Nov 2012
Franneby U, Gunnarsson U, Andersson M, Heuman R, Nordin P, Nyren O, Sandblom G (2008) Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg 95:488–493
Dahlstrand U, Sandblom G, Nordin P, Wollert S, Gunnarsson U (2011) Chronic pain after femoral hernia repair: a cross-sectional study. Ann Surg 254:1017–1021
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Wright D, Paterson C, Scott N, Hair A, O’Dwyer PJ (2002) Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg 235:333–337
Andersson B, Hallen M, Leveau P, Bergenfelz A, Westerdahl J (2003) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trial. Surgery 133:464–472
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–824
Felix EL, Michas CA, Gonzalez MH Jr (1995) Laparoscopic hernioplasty TAPP vs TEP. Surg Endosc 9:984–989
Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B (2003) Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: a prospective randomized controlled trial. Ann Surg 237:142–147
Kuhry E, van Veen RN, Langeveld HR, Steyerberg EW, Jeekel J, Bonjer HJ (2007) Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc 21:161–166
Acknowledgments
This work was funded by the Uppsala County Council and Stockholm County Council, ALF Grant No. 20100046.
Disclosures
Drs. Ursula Dahlstrand, Gabriel Sandblom, Staffan Wollert, Mikael Ljungdahl, and Ulf Gunnarsson have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dahlstrand, U., Sandblom, G., Ljungdahl, M. et al. TEP under general anesthesia is superior to Lichtenstein under local anesthesia in terms of pain 6 weeks after surgery: results from a randomized clinical trial. Surg Endosc 27, 3632–3638 (2013). https://doi.org/10.1007/s00464-013-2936-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2936-1