Abstract
Background
Current surgical training involves integration of educational interventions together with service requirements during regular working hours. Studies have shown that voluntary training has a low acceptance among surgical trainees and obligatory simulation training during the regular working week leads to better skill acquisition and retention. We examined the difference in training effectiveness depending on the time of day.
Methods
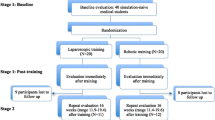
Surgical novices underwent a curriculum consisting of nine basic laparoscopic tasks. The subjects were permitted to choose a training session between during regular working hours (8:00–16:00) or after hours (16:00–20:00). Each subject underwent baseline and post-training evaluation after completion of two 4-h sessions. Task completion was measured in time (s), with penalties for inaccurate performance. Statistical analysis included matched-pairs analysis (sex, age, and previous operative experience) with χ2 und Mann–Whitney U test for between groups and Wilcoxon signed-rank test for testing within one group.
Results
There were no differences in demographic characteristics between the groups. Comparison of the individual baseline and post-training performance scores showed a significant (P < 0.05) improvement for all subjects in all exercises. No significant differences between groups were observed.
Conclusion
All subjects improved in skill significantly throughout the week regardless of the timing of the training intervention. Simulation training can be offered outside of regular working hours with acceptable effectiveness.




Similar content being viewed by others
References
Prystowsky JB (2005) Are young surgeons competent to perform alimentary tract surgery? Arch Surg 140:495–500
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23:622–628
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum 46:1371–1388
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525
Rosser JC Jr, Rosser LE, Savalgi RS (1998) Objective evaluation of a laparoscopic surgical skill program for residents and senior surgeons. Arch Surg 133:657–661
Keyser EJ, Derossis AM, Antoniuk M, Sigman HH, Fried GM (2000) A simplified simulator for the training and evaluation of laparoscopic skills. Surg Endosc 14:149–153
Risucci D, Geiss A, Gellman L, Pinard B, Rosser J (2001) Surgeon-specific factors in the acquisition of laparoscopic surgical skills. Am J Surg 181:289–293
Scott DJ, Young WN, Tesfay ST, Frawley WH, Rege RV, Jones DB (2001) Laparoscopic skills training. Am J Surg 182:137–142
Korndorffer JR Jr, Stefanidis D, Scott DJ (2006) Laparoscopic skills laboratories: current assessment and a call for resident training standards. Am J Surg 191:17–22
Bonrath EM, Buckl L, Bruwer M, Senninger N, Rijcken E (2012) Education in laparoscopic surgery: national survey on current strategies and relevance of simulation training. Zentralbl Chir 137(2):160–164
Schmidt C, Collette F, Cajochen C, Peigneux P (2007) A time to think: circadian rhythms in human cognition. Cogn Neuropsychol 24:755–789
Kvint S, Bassiri B, Pruski A, Nia J, Nemet I, Lopresti M, Perfetti B, Moisello C, Tononi G, Ghilardi MF (2011) Acquisition and retention of motor sequences: the effects of time of the day and sleep. Arch Ital Biol 149:303–312
Bonrath EM, Weber BK, Fritz M, Mees ST, Wolters H, Senninger N, Rijcken E (2012) Laparoscopic simulation training: testing for skill acquisition and retention. Surgery 152(1):12–20
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17:964–967
Vassiliou MC, Ghitulescu GA, Feldman LS, Stanbridge D, Leffondre K, Sigman HH, Fried GM (2006) The MISTELS program to measure technical skill in laparoscopic surgery: evidence for reliability. Surg Endosc 20:744–747
Fried GM, Derossis AM, Bothwell J, Sigman HH (1999) Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator. Surg Endosc 13:1077–1081 discussion 1082
Van Sickle KR, Ritter EM, Smith CD (2006) The pretrained novice: using simulation-based training to improve learning in the operating room. Surg Innov 13:198–204
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463
Edelman DA, Mattos MA, Bouwman DL (2010) FLS skill retention (learning) in first year surgery residents. J Surg Res 163:24–28
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 202:599–603
Chang L, Petros J, Hess DT, Rotondi C, Babineau TJ (2007) Integrating simulation into a surgical residency program: is voluntary participation effective? Surg Endosc 21:418–421
van Dongen KW, van der Wal WA, Rinkes IH, Schijven MP, Broeders IA (2008) Virtual reality training for endoscopic surgery: voluntary or obligatory? Surg Endosc 22:664–667
Uchal M, Tjugum J, Martinsen E, Qiu X, Bergamaschi R (2005) The impact of sleep deprivation on product quality and procedure effectiveness in a laparoscopic physical simulator: a randomized controlled trial. Am J Surg 189:753–757
Tomasko JM, Pauli EM, Kunselman AR, Haluck RS (2012) Sleep deprivation increases cognitive workload during simulated surgical tasks. Am J Surg 203:37–43
Kahol K, Leyba MJ, Deka M, Deka V, Mayes S, Smith M, Ferrara JJ, Panchanathan S (2008) Effect of fatigue on psychomotor and cognitive skills. Am J Surg 195:195–204
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2001) Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ 323:1222–1223
Acknowledgments
This work was funded by a Grant from Rolf Dierichs-Stiftung Muenster 2008 to ER and EB.
Disclosures
Drs. Esther Bonrath, Mathias Fritz, Soeren T. Mees, Barbara K. Weber, Teodor P. Grantcharov, Norbert Senninger, and Emile Rijcken have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonrath, E.M., Fritz, M., Mees, S.T. et al. Laparoscopic simulation training: does timing impact the quality of skills acquisition?. Surg Endosc 27, 888–894 (2013). https://doi.org/10.1007/s00464-012-2529-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2529-4