Abstract
Background
Currently, no guidelines exist for the treatment of patients with multiple colorectal adenomas (MCRAs) (>10 but <100 synchronous nondiminutive polyps of the large bowel). This retrospective study aimed to investigate the clinical and molecular factors related to different treatments for MCRAs.
Methods
Patients with MCRAs were consecutively enrolled from January 2003 to June 2011. Sequencing of their APC and MutYH genes was performed. The clinical, molecular, and family histories of the patients were collected using the Progeny database. The patient treatments were divided into three groups of increasing clinical weight: endoscopic polypectomy, segmental resection, and total colectomy. A logistic regression analysis of clinicomolecular factors related to different treatment options was performed.
Results
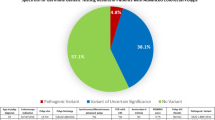
The study comprised 80 patients (32 women, 40 %) with a median age of 53 years (range 13–74 years). The median number of polyps was 33 (range 10–90).The cases included 62 diffuse polyposis, 18 segmental polyposis coli and synchronous colorectal carcinomas (CRC; 34 cases, 43%). The pathogenetic mutations were biallelic MutYH (n = 19, 24 %) and APC (n = 4, 5 %). The mean follow-up period was 74 months (median 43 months, range 1–468 months). Endoscopic polypectomy was performed in 25 cases (31 %), segmental resection in 16 cases (20 %), and total colectomy in 39 cases (49 %). The logistics regression analysis, considering all the patients, showed that the number of polyps, the presence of CRC, and mutation were correlated with more intensive treatment. For the patients without CRC, only the number of polyps was correlated with the severity of the treatment (p > 0.0166). “On the ROC (receiver operating characteristic) curve, 25 was the number of polyps that best discriminated between surgical and endoscopic therapy.
Conclusions
The majority of patients with MCRAs undergo surgery. For patients without CRC, only the number of polyps, and not the presence of a disease-causing mutation, is correlated with increased heaviness of treatment. Patients with more than 25 polyps are more likely to undergo a surgical resection.


Similar content being viewed by others
References
Thliveris A, Samowitz W, Carlson M, Gelbert L, Albertsen H, Joslyn G, Stevens J, Spirio L, Robertson M (1991) Identification and characterization of the familial adenomatous polyposis coli gene. Cell 66:589–600
Phillips RKS, Spigelman AD (1996) Can we safely delay or avoid prophylactic colectomy in familial adenomatous polyposis? Br J Sur 83:769–770
Aziz O, Athanasiou T, Fazio VW, Nicholls RJ, Darzi AW, Church J, Phillips RK, Tekkis PP (2006) Meta-analysis of observational studies of ileorectal versus ileal pouch-anal anastomosis for familial adenomatous polyposis. Br J Surg 93:407–417
Thirlwell C, Howarth KM, Segditsas S, Guerra G, Thomas HJ, Phillips RK, Talbot IC, Gorman M, Novelli MR, Sieber OM, Tomlinson IP (2007) Investigation of pathogenic mechanisms in multiple colorectal adenoma patients without germiline APC or MYH/MUTYH mutation. Br J Cancer 96:1729–1734
Nielsen M, Hes FJ, Nagengast FM, Weiss MM, Mathus-Vliegen EM, Morreau H, Breuning MH, Wijnen JT, Tops CM, Vasen HF (2007) Germline mutations is APC and MUTYH are responsible for the majority of families with attenuated familial adenomatous polyposis. Clin Genet 71:427–433
Sieber OM, Lipton L, Crabtree M, Heinimann K, Fidalgo P, Phillips RK, Bisgaard ML, Orntoft TF, Aaltonen LA, Hodgson SV, Thomas HJ, Tomlinson IP (2003) Multiple colorectal adenomas, classic adenomatous polyposis, and germline mutations in MYH. N Engl J Med 348:791–799
O’Shea AM, Cleary SP, Croitoru MA, Kim H, Berk T, Monga N, Riddell RH, Pollett A, Gallinger S (2008) Pathological features of colorectal carcinomas in MYH-associated polyposis. Histopathology 53:184–194
Knudsen AL, Bisgaard ML, Bülow S (2003) Attenuated familial adenomatous polyposis (AFAP): a review of the literature. Fam Cancer 2:43–55
van der Luijt RB, Vasen HF, Tops CM, Breukel C, Fodde R, Meera Khan P (1995) APC mutation in the alternatively spliced region of exon 9 associated with late-onset familial adenomatous polyposis. Hum Genet 96:705–710
Filipe B, Baltazar C, Albuquerque C, Fragoso S, Lage P, Vitoriano I, Mão de Ferro S, Claro I, Rodrigues P, Fidalgo P, Chaves P, Cravo M, Nobre Leitão C (2009) APC or MUTYH mutations account for the majority of clinically well-characterized families with FAP and AFAP phenotype and patients with more than 30 adenomas. Clin Genet 76:242–255
Wang L, Baudhuin LM, Boardman LA, Steenblock KJ, Petersen GM, Halling KC, French AJ, Johnson RA, Burgart LJ, Rabe K, Lindor NM, Thibodeau SN (2004) MYH mutations in patients with attenuated and classic polyposis and with young-onset colorectal cancer without polyps. Gastroenterology 127:9–16
Al-Tassan N, Chmiel NH, Maynard J, Fleming N, Livingston AL, Williams GT, Hodges AK, Davies DR, David SS, Sampson JR, Cheadle JP (2002) Inherited variants of MYH associated with somatic G:C→T:a mutations in colorectal tumors. Nat Genet 30:227–232
Poulsen ML, Bisgaard ML (2008) MUTYH associated polyposis (MAP). Curr Genomics 9:420–435
Morak M, Laner A, Bacher U, Keiling C, Holinski-Feder E (2010) MUTYH-associated polyposis: variability of the clinical phenotype in patients with biallelic and monoallelic MUTYH mutations and report on novel mutations. Clin Genet 78:353–363
Vasen HF, Möslein G, Alonso A, Aretz S, Bernstein I, Bertario L, Blanco I, Bülow S, Burn J, Capella G, Colas C, Engel C, Frayling I, Friedl W, Hes FJ, Hodgson S, Järvinen H, Mecklin JP, Møller P, Myrhøi T, Nagengast FM, Parc Y, Phillips R, Clark SK, de Leon MP, Renkonen-Sinisalo L, Sampson JR, Stormorken A, Tejpar S, Thomas HJ, Wijnen J (2008) Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut 57:704–713
Nascimbeni R, Pucciarelli S, Di Lorenzo D, Urso E, Casella C, Agostini M, Nitti D, Salerni B (2010) Rectum-sparing surgery may be appropriate for biallelic MutYH-associated polyposis. Dis Colon Rectum 53:1670–1675
Agostini M, Bedin C, Pucciarelli S, Enzo M, Briarava M, Seraglia R, Ragazzi E, Traldi P, Molin L, Urso ED, Mammi I, Viel A, Lise M, Tasciotti E, Biasiolo A, Pontisso P, Nitti D.(2012) APC I1307 K mutations and forkhead box gene (FOXO1A): another piece of an interesting correlation. Int J Biol Markers 27:13–9 doi:10.5301/JBM.2011.8908
Knudsen AL, Bülow S, Tomlinson I, Möslein G, Heinimann K, Christensen IJ; AFAP Study Group (2010) Attenuated familial adenomatous polyposis: results from an international collaborative study. Colorectal Dis 12(10 online):e243–e249
van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E (2006) Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol 101:343–350
Sanaka MR, Deepinder F, Thota PN, Lopez R, Burke CA (2009) Adenomas are detected more often in morning than in afternoon colonoscopy. Am J Gastroenterol 104:1659–1664
Stoffel EM, Turgeon DK, Stockwell DH, Zhao L, Normolle DP, Tuck MK, Bresalier RS, Marcon NE, Baron JA, Ruffin MT, Brenner DE, Syngal S, Great Lakes-New England Clinical Epidemiology and Validation Center of the Early Detection Research Network (2008) Missed adenomas during colonoscopic surveillance in individuals with Lynch syndrome (hereditary nonpolyposis colorectal cancer). Cancer Prev Res 1:470–475
Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P, Potier P, Sautereau D, Boustière C, Grimaud JC, Barthélémy C, Sée J, Serraj I, D’Halluin PN, Branger B, Ponchon T (2008) Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy 40:284–290
Waye JD, Lewis BS, Yessayan S (1992) Colonoscopy: a prospective report of complications. J Clin Gastroenterol 15:347–351
Rex DK, Lewis BS, Waye JD (1992) Colonoscopy and endoscopic therapy for delayed post-polypectomy hemorrhage. Gastrointest Endosc 38:127–129
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual (2010, seventh edition). Retrieved at http://www.cancerstaging.org
Yamamoto S, Watanabe M, Hasegawa H, Baba H, Yoshinare K, Shiraishi J, Kitajima M (2004) The risk of lymph node metastasis in T1 colorectal carcinoma. Hepatogastroenterology 51:998–1000
Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR (2002) Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum 45:200–206
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Parry S, Win AK, Parry B, Macrae FA, Gurrin LC, Church JM, Baron JA, Giles GG, Leggett BA, Winship I, Lipton L, Young GP, Young JP, Lodge CJ, Southey MC, Newcomb PA, Le Marchand L, Haile RW, Lindor NM, Gallinger S, Hopper JL, Jenkins MA (2011) Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 60:950–957
Nascimbeni R, Urso E, Pucciarelli S, et al (2012) High risk of rectal cancer and of metachronous colorectal cancer in probands of families fulfilling Amsterdam criteria. Ann Surg In press
Natarajan N, Watson P, Silva-Lopez E, Lynch HT (2010) Comparison of extended colectomy and limited resection in patients with Lynch syndrome. Dis Colon Rectum 53:77–82
Disclosures
Emanuele D. L. Urso, Riccardo Nascimbeni, Salvatore Pucciarelli, Marco Agostini, Claudio Casella, Dario Moneghini, Diego Di Lorenzo, Isacco Maretto, Maribel Sullivan, Isabella Mammi, Alessandra Viel, and Donato Nitti have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Urso, E.D.L., Nascimbeni, R., Pucciarelli, S. et al. Factors affecting the treatment of multiple colorectal adenomas. Surg Endosc 27, 207–213 (2013). https://doi.org/10.1007/s00464-012-2421-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2421-2