Abstract
Background
The aim of this study is to design a simple, secure, and safe technique of intracorporeal Pringle’s maneuver to facilitate safer laparoscopic liver resection.
Methods
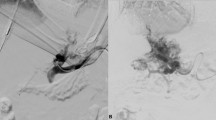
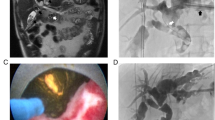
A self-designed six-loop catheter was made using 20-French T-tube and 10-French nelaton urethral catheter. The cross head and stem of the T-tube were trimmed to 1 cm, respectively. The nelaton was shortened to 12-cm-long tube from the round tip, and the cut end was inserted and sutured to the stem of the T-tube. After establishment of pneumoperitoneum, the T-tube with nelaton was placed into the abdomen. The round end of the nelaton was inserted into the lesser sac and pulled through the foramen of Winslow, and the end of nelaton was then inserted into one end of the T-tube and pulled through the other end, forming a six-loop. The nelaton was pulled to occlude the hepatic inflow and temporarily fixed with 1-0 Vicryl on a curved round needle on the other end of the T-tube. The protocol of Pringle’s maneuver was 15-min clamp and 5-min release periods. The liver parenchymal transection was performed using Harmonic scalpel.
Results
From November 2009 to August 2011, 20 patients received laparoscopic liver resection using the six-loop Pringle’s maneuver. During operation, 17 patients were positioned supine, 2 patients in left decubitus, and 1 patient in supine followed by left decubitus position. There were 9 anatomical resections and 11 nonanatomical resections (18 patients for single lesion, 1 for two lesions, and 1 for three lesions). The average times of liver resection and Pringle’s maneuver were 33.1 and 36.2 min, respectively. Mean blood loss was 102.5 ml. The postoperative course was uneventful, and average hospital stay was 4.4 days.
Conclusion
Our self-designed six-loop intracorporeal Pringle’s maneuver can facilitate safer laparoscopic liver resection.



Similar content being viewed by others
References
Shiba H, Ishida Y, Wakiyama S, Iida T, Matsumoto M, Sakamoto T, Ito R, Gocho T, Furukawa K, Fujiwara Y, Hirohara S, Misawa T, Yanaga K (2009) Negative impact of blood transfusion on recurrence and prognosis of hepatocellular carcinoma after hepatic resection. J Gastrointest Surg 13:1636–1642
Man K, Fan ST, Ng IO, Lo CM, Liu CL, Wong J (1997) Prospective evaluation of Pringle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg 226:704–711
Maehara S, Adachi E, Shimada M, Taketomi A, Shirabe K, Tanaka S, Maeda T, Ikeda K, Higashi H, Maehara Y (2007) Clinical usefulness of biliary scope for Pringle’s maneuver in laparoscopic hepatectomy. J Am Coll Surg 205:816–818
Cho A, Yamamoto H, Nagata M, Takiguchi N, Shimada H, Kainuma O, Souda H, Gunji H, Miyazaki A, Ikeda A (2009) Safe and feasible inflow occlusion in laparoscopic liver resection. Surg Endosc 23:906–908
Machado MA, Makdissi FF, Bacchella T, Machado MC (2005) Hemihepatic ischemia for laparoscopic liver resection. Surg Laparosc Endosc Percutan Tech 15:180–183
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250:831–841
Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Vogt D, Fung J, Berber E (2009) Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc 23:847–853
Polignano FM, Quyn AJ, de Figueiredo RS, Henderson NA, Kulli C, Tait IS (2008) Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc 22:2564–2570
Schmandra TC, Mierdl S, Bauer H, Gutt C, Hanisch E (2002) Transoesophageal echocardiography shows high risk of gas embolism during laparoscopic hepatic resection under carbon dioxide pneumoperitoneum. Br J Surg 89:870–876
Min SK, Kim JH, Lee SY (2007) Carbon dioxide and argon gas embolism during laparoscopic hepatic resection. Acta Anaesthesiol Scand 51:949–953
Disclosures
The authors have no conflicts of interest or financial ties to disclosure. There was no funding from commercial device companies or national government grants during the study period. This manuscript was completed by Dr. Ying-Jui Chao and Dr. Yan-Shen Shan. Most of the cases were performed by Dr. Ying-Jui Chao, with Dr. Chih-Jung Wang as first assistant. Dr. Yan-Shen Shan was the supervisor of the other two authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chao, YJ., Wang, CJ. & Shan, YS. Technical notes: a self-designed, simple, secure, and safe six-loop intracorporeal Pringle’s maneuver for laparoscopic liver resection. Surg Endosc 26, 2681–2686 (2012). https://doi.org/10.1007/s00464-012-2210-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2210-y