Abstract
Background
Risk factors for conversion in cholecystectomy may be of clinical value. This study aimed to investigate whether a set of risk factors, including the surgeon’s specialization, can be used for the development of a preoperative strategy to optimize conversion outcome.
Methods
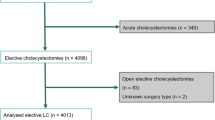
The data for all patients who underwent laparoscopic cholecystectomy at a single institution between January 2004 and December 2008 were retrospectively reviewed. Factors predictive for conversion were identified, and a preoperative strategy model was deduced.
Results
Of the 1,126 patients analyzed, 106 (9%) underwent laparoscopic cholecystectomy in an emergency setting. Delayed surgery was performed for 63 (46%) of 138 patients (12%) with acute cholecystitis. Preoperative endoscopic retrograde cholangiography was achieved for 161 of the patients (14%). Risk factors predictive of conversion (for 65 patients) were male gender [odds ratio (OR), 2.3; 95% confidence interval (CI), 1.3–3.9; p = 0.004], age older than 65 years (OR, 2.6; 95% CI, 1.4–4.8; p = 0.002), body mass index (BMI) exceeding 25 kg/m2 (OR, 3.4; 95% CI, 1.7–7.1; p < 0.001), history of complicated biliary disease (HCBD) (OR, 5.6; 95% CI, 3.2–9.8; p = < 0.001), and surgery by a non-gastrointestinal (non-GI) surgeon (OR, 4.9; 95% CI, 2.2–10.6; p < 0.001). The conversion rate for patients with a history of no complications who had two or more risk factors (gender, age, BMI > 25) and for patients with a HCBD who had one or more risk factors was significantly higher if the surgery was performed by non-GI rather than GI surgeons.
Conclusion
Male gender, age older than 65 years, BMI exceeding 25 kg/m2, HCBD, and surgery by a non-GI surgeon are predictive for conversion. A preoperative triage for surgeon selection based on risk factors and a HCBD is proposed to optimize conversion outcome.


Similar content being viewed by others
References
Adamsen S, Hansen OH, Funch-Jensen P, Schulze S, Stage JG, Wara P (1997) Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg 184:571–578
Alponat A, Kum CK, Koh BC, Rajnakova A, Goh PM (1997) Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg 21:629–633
Ballal M, David G, Willmott S, Corless DJ, Deakin M, Slavin JP (2009) Conversion after laparoscopic cholecystectomy in England. Surg Endosc 23:2338–2344
Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, Goresky CA, Meakins JL (1992) Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill Gallstone Treatment Group. Lancet 340:1116–1119
Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D (1994) Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia, and trauma responses. Br J Surg 81:1362–1365
Boddy AP, Bennett JM, Ranka S, Rhodes M (2007) Who should perform laparoscopic cholecystectomy? A 10-year audit. Surg Endosc 21:1492–1497
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, Boerma EJ, Obertop H, Huibregtse K, Gouma DJ (2002) Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile duct stones: a randomised trial. Lancet 360:761–765
Brodsky A, Matter I, Sabo E, Cohen A, Abrahamson J, Eldar S (2000) Laparoscopic cholecystectomy for acute cholecystitis: can the need for conversion and the probability of complications be predicted? A prospective study. Surg Endosc 14:755–760
Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ (2001) Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc 15:700–705
Chandler CF, Lane JS, Ferguson P, Thompson JE, Ashley SW (2000) Prospective evaluation of early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Am Surg 66:896–900
Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA (2010) Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci 55:2398–2405
Cuschieri A, Dubois F, Mouiel J, Mouret P, Becker H, Buess G, Trede M, Troidl H (1991) The European experience with laparoscopic cholecystectomy. Am J Surg 161:385–387
David GG, Al Sarira AA, Willmott S, Deakin M, Corless DJ, Slavin JP (2008) Management of acute gallbladder disease in England. Br J Surg 95:472–476
de Vries A, Donkervoort SC, van Geloven AA, Pierik EG (2005) Conversion rate of laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis: does the time interval matter? Surg Endosc 19:996–1001
Donkervoort SC, van Ruler O, Dijksman LM, van Geloven AA, Pierik EG (2010) Identification of risk factors for an unfavorable laparoscopic cholecystectomy course after endoscopic retrograde cholangiography in the treatment of choledocholithiasis. Surg Endosc 24:798–804
Eldar S, Sabo E, Nash E, Abrahamson J, Matter I (1997) Laparoscopic versus open cholecystectomy in acute cholecystitis. Surg Laparosc Endosc 7:407–414
Gurusamy KS, Samraj K (2006) Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev CD005440
Hasukic S, Mesic D, Dizdarevic E, Keser D, Hadziselimovic S, Bazardzanovic M (2002) Pulmonary function after laparoscopic and open cholecystectomy. Surg Endosc 16:163–165
Hendolin HI, Paakonen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P (2000) Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. Eur J Surg 166:394–399
Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M (2001) A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg 181:520–525
Kauvar DS, Braswell A, Brown BD, Harnisch M (2006) Influence of resident and attending surgeon seniority on operative performance in laparoscopic cholecystectomy. J Surg Res 132:159–163
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev CD006231
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus small-incision cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev CD006229
Kortram K, Reinders JS, van Ramshorst B, Wiezer MJ, Go PM, Boerma D (2010) Laparoscopic cholecystectomy for acute cholecystitis should be performed by a laparoscopic surgeon. Surg Endosc 24(9):2206–2209
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188:205–211
Low SW, Iyer SG, Chang SK, Mak KS, Lee VT, Madhavan K (2009) Laparoscopic cholecystectomy for acute cholecystitis: safe implementation of successful strategies to reduce conversion rates. Surg Endosc 23(11):2424–2429
MacFadyen BV Jr, Vecchio R, Ricardo AE, Mathis CR (1998) Bile duct injury after laparoscopic cholecystectomy: the United States experience. Surg Endosc 12:315–321
McManus PL, Wheatley KE (2003) Consent and complications: risk disclosure varies widely between individual surgeons. Ann R Coll Surg Engl 85:79–82
Murphy MM, Ng SC, Simons JP, Csikesz NG, Shah SA, Tseng JF (2010) Predictors of major complications after laparoscopic cholecystectomy: surgeon, hospital, or patient? J Am Coll Surg 211:73–80
Rosen M, Brody F, Ponsky J (2002) Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 184:254–258
Russell JC, Walsh SJ, Reed-Fourquet L, Mattie A, Lynch J (1998) Symptomatic cholelithiasis: a different disease in men? Connecticut Laparoscopic Cholesystectomy Registry. Ann Surg 227:195–200
Sarli L, Iusco DR, Roncoroni L (2003) Preoperative endoscopic sphincterotomy and laparoscopic cholecystectomy for the management of cholecystocholedocholithiasis: 10-year experience. World J Surg 27:180–186
Shea JA, Healey MJ, Berlin JA, Clarke JR, Malet PF, Staroscik RN, Schwartz JS, Williams SV (1996) Mortality and complications associated with laparoscopic cholecystectomy: a meta-analysis. Ann Surg 224:609–620
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystectomy to open surgery. JSLS 10:359–363
Disclosure
Sandra C. Donkervoort, Lea M. Dijksman, Lincey C.F. de Nes, Pieter G. Versluis, Joris Derksen, and Michael F. Gerhards have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donkervoort, S.C., Dijksman, L.M., de Nes, L.C.F. et al. Outcome of laparoscopic cholecystectomy conversion: is the surgeon’s selection needed?. Surg Endosc 26, 2360–2366 (2012). https://doi.org/10.1007/s00464-012-2189-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2189-4