Abstract
Introduction
Perioperative anticancer therapy that does not impair wound healing is needed to counter the persistent proangiogenic plasma compositional changes that occur after colorectal resection. Polyphenon E (PolyE), a green tea derivative (main component EGCG), and Siliphos (main component silibinin), from the milk thistle plant, both have antitumor effects. This study assessed the impact of PolyE/Siliphos (PES) on wound healing and the growth of CT-26 colon cancer in several murine models.
Methods
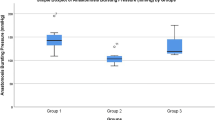
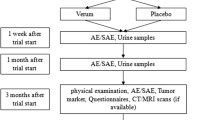
One wound healing and three tumor studies were performed. Tumor Study (TS)1 assessed the impact of PES on subcutaneous tumor growth, whereas TS2 assessed PES’s impact on subcutaneous growth when given pre- and post-CO2 pneumoperitoneum (pneumo), sham laparotomy, or anesthesia alone. TS3 determined the ability of PES to limit hepatic metastases (mets) after portal venous injection of tumor cells. In the final study, laparotomy and gastrotomy wound healing were assessed several ways. BALB/c mice were used for all studies. The drugs were given via drinking water (PolyE) and gavage (Siliphos), daily, for 7–9 days preprocedure and for 7–21 days postoperatively. Tumor mass, number/size of hepatic mets, and proliferation and apoptosis rates were assessed. The abdominal breaking strength and energy to failure were measured postmortem as was gastric bursting pressures.
Results
PES significantly inhibited subcutaneous growth in the nonoperative setting. PES also significantly decreased the number/size of liver mets when given perioperatively. Abdominal wound breaking strength, energy to wound failure, and collagen content were not altered by PES; gastrotomy bursting strength also was not affected by PES. Neither drug alone had a significant impact on tumor growth.
Conclusions
The PES combination inhibited subcutaneous and hepatic tumor growth yet did not impair wound healing. PES holds promise as a perioperative anticancer therapy.










Similar content being viewed by others
References
DeVita H, Rosenberg (2005) DeVita, Hellman, and Rosenberg’s cancer. In: Principles and practice of oncology, 8th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1061–1125
Weese JL, Ottery FD, Emoto SE (1986) Do operations facilitate tumor growth? An experimental model in rats. Surgery 100(2):273–277
Allendorf JD, Bessler M, Kayton ML, Oesterling SD, Treat MR, Nowygrod R, Whelan RL (1995) Increased tumor establishment and growth after laparotomy vs. laparoscopy in a murine model. Arch Surg 130(6):649–653
Allendorf JD, Bessler M, Horvath KD, Marvin MR, Laird DA, Whelan RL (1999) Increased tumor establishment and growth after open vs. laparoscopic surgery in mice may be related to differences in postoperative T-cell function. Surg Endosc 13(3):233–235
Wildbrett P, Oh A, Carter JJ, Schuster H, Bessler, Jaboci CA, Whelan RL (2002) Increased rates of pulmonary metastases following sham laparotomy compared to CO2 pneumoperitoneum and the inhibition of metastases utilizing perioperative immunomodulation and a tumor vaccine. Surg Endosc 16(8):1162–1169
Kumara HM, Feingold D, Kalady M, Dujovny N, Senagore A, Hyman A, Cekic V, Whelan RL (2009) Colorectal resection is associated with persistent proangiogenic plasma protein changes: postoperative plasma stimulates in vitro endothelial cell growth, migration, and invasion. Ann Surg 249(6):973–977
Morris T, Lincoln F, Lee A (1978) The effect of 5-fluorouracil on abdominal wound healing in rats. Aust N Z J Surg 48(2):219–221
Weiber S, Graf W, Glimelius B, Jiborn H, Pahlman L, Zederfeldt B (1994) The effect of 5-fluorouracil on wound healing and collagen synthesis in left colon anastomoses. An experimental study in the rat. Eur Surg Res 26(3):173–178
Shukla VK, Pandey M, Das PC, Tiwary SK, Chansouria JP, Kumar M, Singh G, Pandey SK, Singh G (2007) Effect of 5-fluorouracil and mitomycin on the healing of intestinal anastomosis. Chemotherapy 53(4):275–281
Ozel L, Ozel MS, Toros AB, Kara M, Ozkan KS, Tellioglu G, Krand O, Koyuturk M, Berber I (2009) Effect of early preoperative 5-fluorouracil on the integrity of colonic anastomoses in rats. World J Gastroenterol 15(33):4156–4162
Bode AM, Dong Z (2009) Epigallocatechin 3-gallate and green tea catechins: united they work, divided they fail. Cancer Prev Res 2(6):514–517
Hwang JT, Ha J, Park IJ, Lee SK, Baik HW, Kim YM, Park OJ (2007) Apoptotic effect of EGCG in HT-29 colon cancer cells via AMPK signal pathway. Cancer Lett 247(1):115–121
Shimizu M, Deguchi A, Hara Y, Moriwaki H, Weinstein IB (2005) EGCG inhibits activation of the insulin-like growth factor-1 receptor in human colon cancer cells. Biochem Biophys Res Comm 334(3):947–953
Shimizu M, Shirakami Y, Sakai H, Adachi S, Hata K, Hirose Y, Tsurumi H, Tanaka T, Moriwaki H (2008) (−)-Epigallocatechin gallate suppresses azoxymethane-induced colonic premalignant lesions in male C57BL/KsJ-db/db mice. Cancer Prev Res 1(4):298–304
Yuan JH, Li YQ, Yang XY (2008) Protective effects of epigallocatechin gallate on colon preneoplastic lesions induced by 2-amino-3-methylimidazo[4,5-f]quinoline in mice. Mol Med 14(9–10):590–598
Saller R, Brignoli R, Melzer J, Meier R (2008) An updated systematic review with meta-analysis for the clinical evidence of silymarin. Forschende Komplementarmedizin 15(1):9–20
Flora K, Hahn M, Rosen H, Benner K (1998) Milk thistle (Silybum marianum) for the therapy of liver disease. Am J Gastroenterol 93(2):139–143
Wellington K, Jarvis B (2001) Silymarin: a review of its clinical properties in the management of hepatic disorders. Bio Drugs 15(7):465–489
Singh RP, Deep G, Chittezhath M, Kaur M, Dwyer-Nield LD, Malkinson AM, Agarwal R (2006) Effect of silibinin on the growth and progression of primary lung tumors in mice. J Natl Cancer Inst 98(12):846–855
Singh RP, Tyagi A, Sharma G, Mohan S, Agarwal R (2008) Oral silibinin inhibits in vivo human bladder tumor xenograft growth involving down-regulation of survivin. Clin Cancer Res 14(1):300–308
Cui W, Gu F, Hu KQ (2009) Effects and mechanisms of silibinin on human hepatocellular carcinoma xenografts in nude mice. World J Gastroenterol 15(16):1943–1950
Deep G, Raina K, Singh RP, Oberlies NH, Kroll DJ, Agarwal R (2008) Isosilibinin inhibits advanced human prostate cancer growth in athymic nude mice: comparison with silymarin and silibinin. Int J Cancer 123(12):2750–2758
Singh RP, Gu M, Agarwal R (2008) Silibinin inhibits colorectal cancer growth by inhibiting tumor cell proliferation and angiogenesis. Cancer Res 68(6):2043–2050
Kaur M, Velmurugan B, Tyagi A, Agarwal C, Singh RP, Agarwal R (2010) Silibinin suppresses growth of human colorectal carcinoma SW480 cells in culture and xenograft through down-regulation of beta-catenin-dependent signaling. Neoplasia 12(5):415–424
Khan N, Afaq F, Saleem M, Ahmad N, Mukhtar H (2006) Targeting multiple signaling pathways by green tea polyphenol (−)-epigallocatechin-3-gallate. Cancer Res 66(5):2500–2505
Ramasamy K, Agarwal R (2008) Multitargeted therapy of cancer by silymarin. Cancer Lett 269(2):352–362
Ko J, Ross J, Awad H, Hurwitz H, Klitzman B (2005) The effects of ZD6474, an inhibitor of VEGF signaling, on cutaneous wound healing in mice. J Surg Res 129(2):251–259
DuBay DA, Wang X, Adamson B, Kuzon WM Jr, Dennis RG, Franz MG (2005) Progressive fascial wound failure impairs subsequent abdominal wall repairs: a new animal model of incisional hernia formation. Surgery 137(4):463–471
Singh RP, Mallikarjuna GU, Sharma G, Dhanalakshmi S, Tyagi AK, Chan DC, Agarwal C, Agarwal R (2004) Oral silibinin inhibits lung tumor growth in athymic nude mice and forms a novel chemo combination with doxorubicin targeting nuclear factor kappaB-mediated inducible chemoresistance. Clin Cancer Res 10:8641–8647
Shanafelt TD, Call TG, Zent CS, LaPlant B, Bowen DA, Roos M, Secreto CR, Ghosh AK, Kabat BF, Lee MJ, Yang CS, Jelinek DF, Erlichman C, Kay NE (2009) Phase I trial of daily oral polyphenon E in patients with asymptomatic Rai stage 0 to II chronic lymphocytic leukemia. J Clin Oncol 27:3808–3814
Hikino H, Kiso Y, Wagner H, Fiebig M (1984) Anti-hepatotoxic actions of flavonolignans from Silybum marianum fruits. Planta Med 50:248–250
Indena (1992) IdB-1016 silybin phosphatidylcholine complex update. Drugs Future 17:248
Marena C, Lampertico M (1991) Preliminary clinical development of silipide: a new complex of silybin in toxic liver disorders. Planta Med 57:A124–A125
Flaig TW, Glode M, Gustafson D, van Bokhoven A, Tao Y, Wilson S, Su LJ, Li Y, Harrison G, Agarwal R, Crawford ED, Lucia MS, Pollak M (2010) A study of high-dose oral silybin-phytosome followed by prostatectomy in patients with localized prostate cancer. Prostate 70:848–855
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey JN, Nagorney DM, McWilliams RR (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27:3677–3683
Acknowledgement
This project was funded by Society of American Gastrointestinal and Endoscopic Surgeons (SAGES, grant #2009043). We greatly appreciate the support.
Disclosures
Xiaohong Yan, Thomas R. Gardner, Michael Grieco, Sonali A.C. Herath, Joon Ho Jang, Daniel Kirchoff, Linda Njoh, H.M.C. Shantha Kumara, Samer Naffouje, and Richard L. Whelan have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, X., Gardner, T.R., Grieco, M. et al. Perioperative polyphenon E- and siliphos-inhibited colorectal tumor growth and metastases without impairment of gastric or abdominal wound healing in mouse models. Surg Endosc 26, 1856–1864 (2012). https://doi.org/10.1007/s00464-011-2114-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-2114-2