Abstract
Background
Trocar entry points have been identified as a significant source of pain after laparoscopic surgery. This is particularly true of the larger 12-mm ports that require deep fascial closure to avoid port-site herniation. We investigated whether using radially expanding trocars not requiring fascial closure compared to conventional cutting trocars for the 12-mm port in transabdominal preperitoneal (TAPP) hernia repairs had any effect on postoperative analgesic requirements and return to work or normal activity.
Methods
The number of days analgesia was required postoperatively and the number of days taken to return to normal activity was recorded for 143 consecutive patients who underwent TAPP hernia repair by a single experienced laparoscopic surgeon. Exactly the same operative technique was used in these patients with the exception of the 12-mm port site entry. In group 1 (104 patients), a conventional cutting trocar was used requiring deep fascial closure. In group 2 (39 patients), a radially expanding trocar was used and the fascial defect was not closed.
Results
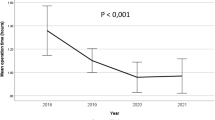
Analgesia was required for an average of 10.5 days in group 1 and 2.4 days in group 2 (P < 0.001). The average time to return to work or to normal activity was 23.4 days in group 1 and 15.6 days in group 2 (P = 0.004). There was no significant difference between the two groups with respect to the patients’ age, sex, or operating time.
Conclusion
Using the laparoscopic TAPP hernia repair as a standardised operation, changing from 12-mm fascial port closure to a technique that uses port dilation (not requiring a potentially “tight” deeper fascial closure) in a similar group of patients shows that there is a significant reduction in postoperative analgesic requirement and an earlier return to productive work or normal lifestyle. Perhaps dilating ports should replace those larger 10-, 12-, and 15-mm ports that require deeper sutures in all laparoscopic surgical operations.


Similar content being viewed by others
References
Lau H, Brooks DC (2001) Predictive factors for unanticipated admissions after ambulatory laparoscopic cholecystectomy. Arch Surg 136:1150–1153
Fiorillo MA, Davidson PG, Fiorillo M, D’Anna JA Jr, Sithian N, Silich RJ (1996) 149 Ambulatory laparoscopic cholecystectomies. Surg Endosc 10:52–56
Bisgaard T, Klarskov B, Rosenberg J, Kehlet H (2001) Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain 90:261–269
Vilos GA, Ternamian A, Dempster J, Laberge PY (2007) Laparoscopic entry: a review of techniques, technologies, and complications. J Obstet Gynaecol Cancer 29:433–465
Durai R, Ng PC (2009) Novel methods of closing 10-mm laparoscopic port-site wounds. J Laparoendosc Adv Surg Technol A 19:791–793
Leibl BJ, Schmedt CG, Schwarz J, Kraft K, Bittner R (1999) Laparoscopic surgery complications associated with trocar tip design: review of literature and own results. J Laparoendosc Adv Surg Technol A 9:135–140
Kadar N, Reich H, Liu CY, Manko GF, Gimpelson R (1993) Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol 168:1493–1495
Bhoyrul S, Mori T, Way LW (1996) Radially expanding dilatation. A superior method of laparoscopic trocar access. Surg Endosc 10:775–778
Turner DJ (1996) A new, radially expanding access system for laparoscopic procedures versus conventional cannulas. J Am Assoc Gynecol Laparosc 3:609–615
Bisgaard T, Jakobsen HL, Jacobsen B, Olsen SD, Rosenberg J (2007) Randomized clinical trial comparing radially expanding trocars with conventional cutting trocars for the effects on pain after laparoscopic cholecystectomy. Surg Endosc 21:2012–2016
Bhoyrul S, Payne J, Steffes B, Swanstrom L, Way LW (2000) A randomized prospective study of radially expanding trocars in laparoscopic surgery. J Gastrointest Surg 4:392–397
Lam TY, Lee SW, So HS, Kwok SP (2000) Radially expanding trocar: a less painful alternative for laparoscopic surgery. J Laparoendosc Adv Surg Technol A 10:269–273
Yim SF, Yuen PM (2001) Randomized double-masked comparison of radially expanding access device and conventional cutting tip trocar in laparoscopy. Obstet Gynecol 97:435–438
Tarnay CM, Glass KB, Munro MG (1999) Entry force and intra-abdominal pressure associated with six laparoscopic trocar-cannula systems: a randomized comparison. Obstet Gynecol 94:83–88
Shekarriz B, Gholami SS, Rudnick DM, Duh QY, Stoller ML (2001) Radially expanding laparoscopic access for renal/adrenal surgery. Urology 58:683–687
Disclosures
Simon Mordecai, Oliver Warren, and Stephen Warren have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mordecai, S.C., Warren, O.W.N. & Warren, S.J. Radially expanding laparoscopic trocar ports significantly reduce postoperative pain in all age groups. Surg Endosc 26, 843–846 (2012). https://doi.org/10.1007/s00464-011-1963-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1963-z