Abstract
Background
The aim of this analysis was to determine the impact of complicated and uncomplicated diverticulitis on conversion rates and complications in patients undergoing laparoscopic surgery (LS) for diverticular disease.
Methods
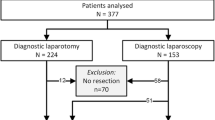
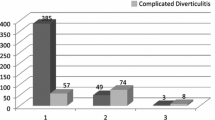
Between 1993 and 2004, 125 patients underwent LS [91 laparoscopic-assisted (LA) and 34 hand-assisted (HA) colectomy for diverticular disease, 79 uncomplicated and 46 complicated]. Cases not completed laparoscopically were considered converted. Complicated diverticulitis was defined as diverticular disease associated with abscess, fistula, bleeding or stricture.
Results
The mean age was 59 years with 67 (54%) men with a mean follow-up of 23 months. The conversion rate was 26% (33 patients). The only factor independently associated with conversion was a history of previous abdominal surgery (37% vs. 14%, p = 0.004). Among the subset of patients undergoing surgery for uncomplicated diverticulitis, the number of diverticulitis episodes (DE), the time between the first and last DE, and the time between the last DE and surgery, were not significantly associated with conversion. Early complications (<30 days from surgery) occurred in 30 (25%) patients. Twenty-one long-term complications (>30 days from surgery) occurred in 20 patients and the one and two-year cumulative probabilities of these complications were 14% and 22%, respectively. Early complications were significantly higher among patients requiring conversion (44% vs. 24%, p = 0.04) but were not significantly higher among patients with complicated diverticulitis (39% vs. 24%, p = 0.11). The rates of long-term complications were not significantly higher among patients that required conversion or had complicated diverticulitis (one-year rate 23% vs. 11%, p = 0.47; 18% vs. 13%, p = 0.70).
Conclusions
A previous history of abdominal surgery was associated with a higher conversion rate in patients undergoing laparoscopic surgery for diverticular disease. Long-term patient outcomes are not adversely impacted by laparoscopic surgery for complicated diverticulitis or laparoscopic surgery requiring conversion to an open procedure.
Similar content being viewed by others
References
Chapman J, et al. (2005) Complicated diverticulitis: is it time to rethink the rules? Ann Surg 242(4): 576–581; discussion 581–583
McConnell EJ, Tessier DJ, Wolff BG (2003) Population-based incidence of complicated diverticular disease of the sigmoid colon based on gender and age. Dis Colon Rectum 46(8): 1110–1114
RobertsP, et al. (1995) Practice parameters for sigmoid diverticulitis. The Standards Task Force American Society of Colon and Rectal Surgeons. Dis Colon Rectum 38(2): 125–132
Eijsbouts QA, et al. (1997) Elective laparoscopic-assisted sigmoid resection for diverticular disease. Surg Endos 11(7): 750–753
Kockerling F, et al. (1999) Laparoscopic resection of sigmoid diverticulitis. Results of a multicenter study. Laparoscopic Colorectal Surgery Study Group. Surg Endos 13(6): 567–571
Plasencia G, et al. (1994) Laparoscopic-assisted sigmoid colectomy and low anterior resection. DisColon Rectum 37(8): 829–833
Trebuchet G Lechaux D, Lecalve JL (2002) Laparoscopic left colon resection for diverticular disease. Surg Endos 16(1): 18–21
Tuech JJ, et al. (2000) Laparoscopic vs open colectomy for sigmoid diverticulitis: a prospective comparative study in the elderly. Surg Endos 14(11): 1031–1033
Sher ME, et al. (1997) Laparoscopic surgery for diverticulitis. Surg Endos 11(3): 264–267
Bouillot JL, et al. (1998) Elective laparoscopic-assisted colectomy for diverticular disease. A prospective study in 50 patients. Surg Endos 12(12): p. 1393–1396
Scheidbach H, et al. (2004) Laparoscopic approach to treatment of sigmoid diverticulitis: changes in the spectrum of indications and results of a prospective, multicenter study on 1,545 patients. DisColon Rectum 47(11): 1883–1888
Vargas HD, et al. (2000) Defining the role of laparoscopic-assisted sigmoid colectomy for diverticulitis. Dis Colon Rectum 43(12): 1726–1731
Franklin ME Jr, et al. (1997) Is laparoscopic surgery applicable to complicated colonic diverticular disease? Surg Endos 11(10): 1021–1025
Gervaz P, et al. (2001) Converted laparoscopic colorectal surgery. Surg Endos 15(8): 827–832
Schwandner O, et al. (2004) Laparoscopic colectomy for recurrent and complicated diverticulitis: a prospective study of 396 patients. Langenbecks Arch Surg 389(2): 97–103
Bartus CM, et al. (2005) Colovesical fistula: not a contraindication to elective laparoscopic colectomy. Dis Colon Rectum 48(2): 233–236
Tekkis PP, Senagore AJ, Delaney CP (2005) Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endos 19(1): 47–54
Bouillot JL, et al. (2002) Elective laparoscopic colonic resection for diverticular disease: results of a multicenter study in 179 patients. Surg Endos 16(9): 1320–1323
Le Moine MC, et al. (2003) Factors and consequences of conversion in laparoscopic sigmoidectomy for diverticular disease. Br J Surg 90(2): 232–236
Laurent SR, et al. (2005) Laparoscopic sigmoidectomy for fistulized diverticulitis. Dis Colon Rectum 48(1): 148–152
Menenakos E, et al. (2003) Laparoscopic surgery for fistulas that complicate diverticular disease. Langenbecks Arch Surg 388(3): 189–193
Natarajan S, Ewings EL, Vega RJ (2004) Laparoscopic sigmoid colectomy after acute diverticulitis: when to operate? Surgery 136(4): 725–730
Slim K, et al. (1995) High morbidity rate after converted laparoscopic colorectal surgery. Br J Surg 82(10):1406–1408
Marusch F, et al. (2001) Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum 44(2): 207–214; discussion 214–216
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in parts at the Society of American Gastrointestinal and Endoscopic Surgeons, Dallas, TX, April 2006; the 10th World Congress of Endoscopic Surgery, Berlin, Germany, September 2006; and the Annual meeting of the Association of Coloproctology of Great Britain and Ireland, Newcastle, England, July 2006
Rights and permissions
About this article
Cite this article
Hassan, I., Cima, R.R., Larson, D.W. et al. The Impact of Uncomplicated and Complicated Diverticulitis on Laparoscopic Surgery Conversion Rates and Patient Outcomes . Surg Endosc 21, 1690–1694 (2007). https://doi.org/10.1007/s00464-007-9413-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9413-7