Abstract
Background
Anterior fundoplication (AF) following laparoscopic Heller myotomy (LHM) for achalasia may prevent esophageal leaks and gastroesophageal reflux but cause dysphagia. Our study attempts to determine the effect of AF on esophageal leaks, nuclear medicine esophageal clearance (EC), symptom frequency (SF), and Van Trappen symptom scores (SS) for dysphagia, regurgitation, and heartburn.
Methods
Between 1995 and 2004, pre- and postoperative (2–12 months) EC, SF, and SS scores were compared in 95 patients undergoing LHM for achalasia with AF (n = 71) and without (n = 24) AF.
Results
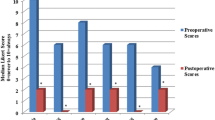
There were no leaks or deaths. Laparoscopic Heller myotomy decreased the frequency of postoperative dysphagia, regurgitation, and heartburn with AF (96% preoperation versus 6% postoperation, 94% versus 3%, 58% versus 6%) (p = 0.001) and without AF (100% versus 0%, 83% versus 0%, 50% versus 4%) (p = 0.001). Laparoscopic Heller myotomy improved all SS in both groups. There was no difference between postoperative dysphagia (1.38 ± 0.64 versus 1.17 ± 38) p = 0.06, regurgitation (1.17 ± 51 versus 1.04 ± 0.20) p = 0.08, and heartburn (1.29 ± 62 versus 1.53 ± 0.80) p = 0.185 scores between the AF and no-AF group, respectively. There is a trend toward improvement in dysphagia and regurgitation in the no-AF group. Laparoscopic Heller myotomy improved EC in the supine and upright positions in both groups of patients (p = 0.001). There was an improved mean change in EC (10 min upright) in the no-AF group versus the AF group (50.7% ± 30.8 versus 29.7% ± 30.2) p = 0.004.
Conclusions
Laparoscopic Heller myotomy improves esophageal transit and the frequency and severity of dysphagia, heartburn, and regurgitation in a safe manner. Patients without AF show a statistically better upright EC with a trend toward improved dysphagia and regurgitation.





Similar content being viewed by others
References
Bonavina L, Nosadini A, Bardini R, Baessato M, Peracchia A (1992) Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg 127:222–227
Castell D, Castell J, eds. (1994) Esophageal Motility Testing, 2nd Edn. Norwalk, CT, Appleton & Lange
Csendes A, Velasco N, Braghetto I, Henriquez A (1981) A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology 80:789–795
Holloway R, Krosin G, Lange R, Baue A, McCallum R (1983) Radionuclide esophageal emptying of a solid meal to quantitate results of therapy in achalasia. Gastroenterology 84:771–776
Malthaner RA, Tood TR, Miller L, Pearson FG (1994) Long-term results in surgically managed esophageal achalasia. Ann Thorac Surg 58:1343–1346; discussion 1346–1347
Pandolfo N, Bortolotti M, Bozzano PL, Mattioli FP (1996) Manometric assessment of Heller-Dor operation for esophageal achalasia. Hepatogastroenterology 43:160–166
Pasricha P, Rai R, Ravich W, Hendrix T, Kalloo A (1996) Botulism toxin for achalasia: long-term outcome and predictors of response. Gastroenterology 110:1410–1415
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Urs D, Eubanks TR, Way LW (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230:587–593; discussion 593–594
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240:405–412; discussion 412–415
Swanstrom LL, Pennings J (1995) Laparoscopic esophagomyotomy for achalasia. Surg Endosc 9:286–290; discussion 290–292
Tatsch K, Schroettle W, Kirsch CM (1991) Multiple swallow test for the quantitative and qualitative evaluation of esophageal motility disorders. J Nucl Med 32:1371–1374
Topart P, Deschamps C, Taillefer R, Duranceau A (1992) Long-term effect of total fundoplication on the myotomized esophagus. Ann Thorac Surg 54:1046–1051
Van Trappen G, Hellemans J (1980) Treatment of achalasia and related motor disorders. Gastroenterology 79:144–154
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finley, C., Clifton, J., Yee, J. et al. Anterior fundoplication decreases esophageal clearance in patients undergoing Heller myotomy for achalasia. Surg Endosc 21, 2178–2182 (2007). https://doi.org/10.1007/s00464-007-9327-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9327-4