Abstract
Background
This study aimed to compare the outcomes for Heller myotomy alone and combined with different partial fundoplications.
Methods
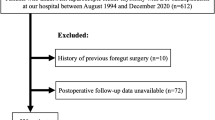
The authors retrospectively reviewed their experience with 69 laparoscopic myotomies and 14 Heller myotomies, 80% of which were performed with partial fundoplication including 20 Toupet, 18 Dor, and 17 modified Dor procedures, in which the fundoplication is sutured to both sides of the crura and not the myotomy.
Results
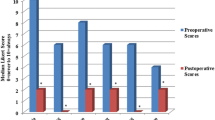
The mean age of the study patients was 69 years (range, 15–80 years). Four mucosal perforations were repaired intraoperatively. There was one small bowel fistula in an area of open hernia repair distant from the myotomy. One patient with severe chronic obstructive pulmonary disease died of pneumonia. Phone follow-up evaluation was achieved in 68% of the cases at a mean of 37 months (range, 2–97 months). The results for no dysphagia and for heartburn requiring proton pump inhibitors, respectively, were as follows: Heller myotomy (85.7%, 28.5%), Toupet (66.6%, 33.3%), Dor (83.3%, 20%), and modified Dor (84.6%, 15.3%). Two patients with reflux strictures required annual dilation (Toupet, Dor). Two patients required revisions: one redo Heller myotomy (Dor) and one esophageal replacement (Toupet).
Conclusion
Heller myotomy provides excellent dysphagia relief with or without fundoplication. Heartburn is a significant problem for a minority of patients. In the authors’ hands, Toupet had the worst results and modified Dor was most protective for heartburn.

Similar content being viewed by others
References
Arain MA, Peters JH, Tamhankar AP, Portale G, Almogy G, DeMeester SR, Crookes PF, Hagen JA, Bremner CG, DeMeester TR (2004) Preoperative lower esophageal sphincter pressure affects outcome of laparoscopic esophageal myotomy for achalasia. J Gastrointest Surg 8: 328–334
Csendes A, Braghetto I, Henriquez A, Cortes C (1989) Late results of a prospective randomised study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 30: 299–304
Decker G, Borie F, Bouamrirene D, Veyrac M, Guillon F, Fingerhut A, Millat B (2002) Gastrointestinal quality of life before and after laparoscopic Heller myotomy with partial posterior fundoplication. Ann Surg 236: 750–758, discussion 758
Dempsey DT, Delano M, Bradley K, Kolff J, Fisher C, Caroline D, Gaughan J, Meilahn JE, Daly JM (2004) Laparoscopic esophagomyotomy for achalasia: does anterior hemifundoplication affect clinical outcome? Ann Surg 239: 779–785, discussion 785–787
Falkenback D, Johansson J, Oberg S, Kjellin A, Wenner J, Zilling T, Johnsson F, Von Holstein CS, Walther B (2003) Heller’s esophagomyotomy with or without a 360 degrees floppy Nissen fundoplication for achalasia: long-term results from a prospective randomized study. Dis Esophagus 16: 284–290
Frantzides CT, Moore RE, Carlson MA, Madan AK, Zografakis JG, Keshavarzian A, Smith C (2004) Minimally invasive surgery for achalasia: a 10-year experience. J Gastrointest Surg 8: 18–23
Mayberry JF, Rhodes J (1980) Achalasia in the city of Cardiff from 1926 to 1977. Digestion 20: 248–252
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138: 490–495, discussion 495–497
Patti MG, Fisichella PM, Perretta S, Galvani C, Gorodner MV, Robinson T, Way LW (2003) Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196: 698–703, discussion 703–705
Raftopoulos Y, Landreneau RJ, Hayetian F, Papasavas P, Naunheim KS, Hazelrigg SR, Santos R, Gagne D, Caushaj P, Keenan RJ (2004) Factors affecting quality of life after minimally invasive Heller myotomy for achalasia. J Gastrointest Surg 8: 233–239
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240: 405–412, discussion 412–415
Richardson WS, Hunter JG (1999) The “floppy” Nissen fundoplication is a completely competent antireflux valve. Surg Endosc 13: 142–145
Richardson WS, Willis GW, Smith JW (2003) Evaluation of scar formation after botulinum toxin injection or forced balloon dilation to the lower esophageal sphincter. Surg Endosc 17: 696–698
Zaninotto G, Annese V, Costantini M, Del Genio A, Costantino M, Epifani M, Gatto G, D’Onofrio V, Benini L, Contini S, Molena D, Battaglia G, Tardio B, Andriulli A, Ancona E (2004) Randomized controlled trial of botulinum toxin versus laparoscopic heller myotomy for esophageal achalasia. Ann Surg 239: 364–370
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Richardson, W.S., Kennedy, C.I. & Bolton, J.S. Midterm follow-up evaluation after a novel approach to anterior fundoplication for achalasia. Surg Endosc 20, 1914–1918 (2006). https://doi.org/10.1007/s00464-006-0227-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0227-9