Abstract
Background
Endoscopic sphincterotomy and stone extraction are standard procedures for the removal of bile duct stones. Stone recurrence can, however, occur in up to 25% of cases. Risk factors have been poorly defined, but are believed to be related to bile stasis. This study investigated whether an angulated common bile duct (CBD) that may predispose to bile stasis influences symptomatic stone recurrence after successful endoscopic therapy.
Methods
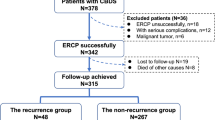
This study included 232 consecutive patients (mean age, 64.1 years; 86 men) who had undergone therapeutic endoscopic retrograde cholangiopancreatography for bile duct stones. Data from the follow-up period (36 ± 17 months) were obtained from medical records and patient questioning. Common bile duct angulation and diameter were measured from the cholangiogram after stone removal.
Results
Symptomatic bile duct stones recurred in 16% of the patients (36/232). Three independent risk factors were identified by multivariate analysis: an angulated CBD (angle, ≤145°; relative risk [RR], 5.2; 95% confidence interval [CI], 2.2–12.5; p = 0.0002), a dilated CBD (diameter, ≥13 mm; RR, 2.6; 95% CI, 1.2–5.7; p = 0.017), and a previous open cholecystectomy (RR, 2.7; 95% CI, 1.3–5.9; p = 0.0117). Gender, age, urgency of procedure, or a periampullary diverticulum did not influence the recurrence rate.
Conclusions
Angulation of the CBD (≤145°) on endoscopic cholangiography, a dilated CBD, and a previous open cholecystectomy are independent risk factors for symptomatic recurrence of bile duct stones. The findings support the role of bile stasis in stone recurrence. Further studies using these data prospectively to identify high-risk patients are warranted.




Similar content being viewed by others
References
Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H (2003) Risk factors for recurrent bile duct stones after endoscopic sphincterotomy. Gut 52: 116–121
Bergman JJ, van der Mey S, Rauws EA, Tijssen JG, Gouma DJ, Tytgat GN, Huibregtse K (1996) Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc 44: 643–649
Costamagna G, Tringali A, Shah SK, Mutignani M, Zucclala G, Perri V (2002) Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy 34: 273–279
Donner A (1984) Approaches to sample size estimation in the design of clinical trials: a review. Stat Med 3: 199–214
Geenen DJ, Geenen JE, Jafri FM, Hogan WJ, Catalano MF, Johnson GK, Schmalz MJ (1998) The role surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Endoscopy 30: 18–20
Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, Park HJ, Joo YH, Yoo KS, Kim HJ, Min YI (2001) Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc 54: 42–48
Lai KH, Lin LF, Lo GH, Cheng JS, Huang RL, Lin CK, Huang JS, Hsu PI, Peng NJ, Ger LP (1999) Does cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? Gastrointest Endosc 49: 483–487
Lai KH, Lo GH, Lin CK, Hsu PI, Chan HH, Cheng JS, Wang EM (2002) Do patients with recurrent choledocholithiasis after endoscopic sphincterotomy benefit from regular follow-up? Gastrointest Endosc 55: 523–526
Lai KH, Peng NJ, Lo GH, Cheng JS, Huang RL, Lin CK, Huang JS, Chiang HT, Ger LP (1997) Prediction of recurrent choledocholithiasis by quantitative cholescintigraphy in patients after endoscopic sphincterotomy. Gut 41: 399–403
Lygidakis NJ (1983) Incidence and significance of primary stones of the common bile duct in choledocholithiasis. Surg Gynecol Obstet 157: 434–436
Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, Adamek HE, Riemann JF (1998) Long-term results (7 to 10 years) of endoscopic sphincterotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc 48: 457–464
Rienmann JF, Lux G, Forster P, Altendorf A (1983) Long-term results after endoscopic sphincterotomy. Endoscopy 15: 165–168
Saito M, Tsuyuguchi T, Yamaguchi T, Ishihara T, Saisho H (2000) Long-term outcome of endoscopic sphincterotomy for choledocholithiasis with cholecystolithiasis. Gastrointest Endosc 51: 540–545
Seifert E (1988) Long-term follow-up after endoscopic sphincterotomy. Endoscopy 20: 232–235
Sugiyama M, Atomi Y (2002) Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 97: 2763–2767
Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y (2004) Endoscopic treatment of recurrent choledocholithiasis after sphincterotomy. Gut 53: 1856–1859
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, Utsunomiya N, Ikeda S (1998) Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc 48: 465–469
Uchiyama K, Onishi H, Tani M, Kinoshita H, Kawai M, Ueno M, Yamaue H (2003) Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg 238: 97–102
Ueno N, Ozawa Y, Aizawa T (2003) Prognostic factors for recurrence of bile duct stones after endoscopic treatment by sphincter dilation. Gastrointest Endosc 58: 336–340
Warren BL (1987) Association between cholangiographic angulation of the common bile duct and choledocholithiasis. South African J Surg 25: 13–15
Acknowledgments
The authors thank Drs. Y. Rattan, A. Hallak, and M. Santo for performing some of the endoscopic procedures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part of this work was presented at the Digestive Disease Week in New Orleans, 16–20 May 2004, and published in abstract form in Gastrointestinal Endoscopy 2004;59: AB197
Rights and permissions
About this article
Cite this article
Keizman, D., Shalom, M.I. & Konikoff, F.M. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc 20, 1594–1599 (2006). https://doi.org/10.1007/s00464-005-0656-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0656-x