Abstract
Background:
The purpose of this research is to compare the wound healing of the laparoscopic esophagomyotomy with and without a gastric patch.
Methods:
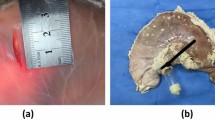
Twelve male pigs were distributed into two groups of six animals. Esophagomyotomy was performed in group A. A gastric patch was associated to the myotomy in group B. On the 21st postoperative day, lumen molding was accomplished to determine the index of stenosis (IS) at the area of myotomy (AM). Macroscopic and microscopic aspects of wound healing were also studied at AM. Three microscopic morphologic patterns were defined for morphometric evaluation: leukocytes (constituted by polymorphonuclear and mononuclear cells), new endothelial cells, and collagen fibers.
Results:
There was a longer operative duration in group B (93.6 min) than in group A (45 min). At AM, IS was negative (lumen increased) and equivalent in both groups: −11.1% in group A and −12.7% in group B. Mesotelial epithelium covering RM was observed in group A. Inflammatory reaction was greater in group B in comparison with group A (leuCocytes: 22 cells versus 8.6; fibrosis: 25.5 fibers versus 15.6; granulation tissue: 18.7 vessels versus 9.7).
Conclusion:
Esophagomyotomy followed by gastric patch does not heal adequately and is worsened by the presence of foreign body granulomas around stitches. Myotomy without gastric patch is faster and causes lower inflammation. Myotomy alone or with gastric patch does not lead to esophageal stenosis at RM and does not lead to restoration of the esophageal musculature continuity.





Similar content being viewed by others
References
Azevedo JLMC, Boulez J (2001) Comparison between laparoscopic esophagocardiomyotomy with and without antireflux procedure in the treatment of achalasia. Surg Endosc 15(Suppl 1): S54
Bloomston M, Boyce W, Mamel J, Albrink M, Murr M, Durkin A, et al. (2000) Videoscopic Heller’s myotomy for achalasia—results beyond short-term follow-up. J Surg Res 92: 150–152
Boulez J, Meeus P, Espalieu P (1997) Oesocardiomyotomie de Heller sans anti-reflux par voie laparoscopique: analyse d’une série de 27 cas. Ann Chir 51: 232–236
Collard JM, Romagnoli R, Lengele B, Salizzoni M, Kenstens PJ (1996) Heller-Dor procedure for achalasia: from conventional to video-endoscopic surgery. Acta Chir Belg 96: 62–65
Delgado F, Bolufer JM, Martinez-Abad M, Martín J, Blanes F, Castro C, et al. (1996) Laparoscopic treatment of esophageal achalasia. Surg Laparosc Endosc 6: 83–90
Dempsey DT, Kalan MMH, Gerson RS, Parkman HP, Maier WP (1999) Comparison of outcomes following open and laparoscopic esophagomyotomy for achalasia. Surg Endosc 13: 747–750
Dor J, Humbert P, Dor V, Figarella J (1962) L’intérêt de la technique de Nissen modifiée dans la prévention du reflux après cardiomyotomie extra-muqueuse de Heller. Mém Acad Chir 88: 877–884
Ellis H, Gibb SP (1975) Reoperation after esophagomyotomy for achalasia of the esophagus. Am J Surg 129: 407–412
Hunter JG, Trus TL, Branum GD, Waring JP (1997) Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg 225: 655–664
Igci A, Müslümanoglu M, Dolay K , Yamaner S, Asoglu O, Avcic C. (1998) Laparoscopic esophagomyotomy without an antireflux procedure for the treatment of achalasia. J Laparoendosc Adv Surg Tech, 8(6): 409–416
Kjellin AP, Granqvist S, Ramel, Thor KBA (1999) Laparoscopic myotomy without fundoplication in patients with achalasia. Eur J Surg 165: 1162–1166
Lyass S, Thoman D, Steiner P, Phillips E (2003) Current status of an antireflux procedure in laparoscopic Heller myotomy. Surg Endosc 17: 554–558
McAdams AJ, Meikle AG, Taylor JO (1970) One layer or two layer colonic anastomoses? Am J Surg 120: 546–550
Mitchell PC, Watson DI, Devitt PG, Briten-Jones R, MacDonald S, Myers JC, et al. (1995) Laparoscopic cardiomyotomy with a Dor patch for achalasia. Can J Surg 38:445–448
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, et al. (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230: 587–593
Peracchia A, Rosati R, Bona S, Fumagalli U, Bonavina L, Chella B (1995) Laparoscopic treatment of functional diseases of the esophagus. Int Surg 80: 336–340
Pinotti HW, Felix VN, Domene CE, Purceli EL (1979) Recurrence of dysphagia in patients operated on for megaesophagus: analysis of determining factors. Chir Gastroenterol 13: 1–7
Raiser F, Perdikis G, Hinder RA, Swanstrom LL, Filipi CJ, McBride PJ, et al. (1996) Heller myotomy via minimal-access surgery: an evaluation of antireflux procedures. Arch Surg 131: 593–597
Richards WO, Sharp KW, Holzman MD (2001) An antireflux procedure should not routinely be added to a Heller myotomy. J Gastrointest Surg 5: 13–16
Robertson GS, Lloyd DM, Wicks AC, Caestecker S, Veitch PS (1995) Laparoscopic Heller’s cardiomyotomy without an antireflux procedure. Br J Surg 82: 957–959
Rosati R, Fumagalli U, Bona S, Bonavina L, Pagani M, Perachia A (1998) Evaluating results of laparoscopic surgery for esophageal achalasia. Surg Endosc 12: 270–273
Wang PC, Sharp KW, Holzman MD, Clements RH, Holcomb GW, Richards WO (1998) The outcome of laparoscopic Heller myotomy without antireflux procedure in patients with achalasia. Am Surg64: 515–521
Yamamura MS, Gilster JC, Myers BS, Denevey CW, Sheppard BC (2000) Laparoscopic Heller myotomy and anterior fundoplication for achalasia results in a high degree of patient satisfaction. Arch Surg 135: 902–906
Acknowledgments
We are grateful for the financial support given by Fundo de Auxílio aos Docentes e Alunos (FADA) from Federal University of São Paulo—Escola Paulista de Medicina and the laparosopic material and equipment given by PCE—Pró-Cirurgia Especializada Ltda—Smith & Nephew, Inc. Parts of this article have been reviewed by Thomas Buckingham, Chief Editor of Life Sciences Publishing, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Azevedo, J., Kozu, F., Azevedo, O. et al. Wound healing of laparoscopic esophageal myotomy with or without an added gastric patch. Surg Endosc 19, 1320–1324 (2005). https://doi.org/10.1007/s00464-004-2082-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-2082-x