Abstract
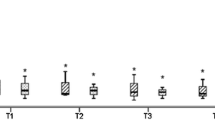
Background: Pneumothorax is a known complication of laparoscopy, with most pneumothoraces diagnosed postoperatively with conventional chest x-ray. Electrocardiogram (ECG) conduction changes are associated with pneumothorax. In a sheep model, ECG changes were evaluated as a potential indicator of intraoperative pneumothorax. Additionally, resolution rates of helium (He) and carbon dioxide (CO2) pneumothorax were also evaluated in this model.Methods: Under general anesthesia, 10 sheep had known volumes (20–100 cc) of either He or CO2 introduced into the left hemithorax. A 12-lead ECG recorded changes associated with the induced pneumothorax. After changes in the ECG plateaued, the gas volume in the hemithorax was increased to 2 L and the resultant pneumothorax was followed for a 2-h period using fluoroscopy to determine resolution rates for the different gas pneumothoraces. Gas volumes were aspirated after 2 h and ECGs were again recorded.Results: Pneumothorax volumes as low as 20 cc produced consistent ECG changes. The amplitude of the precordial QRS complex was seen to diminish, and this lowering of the QRS amplitude continued as pneumothorax volume increased up to 100 cc. The ECG returned to prepneumothorax patterns with aspiration of the left chest. For different gas pneumothoraces, CO2 pneumothorax showed almost complete resolution in the 2-h period, whereas He pneumothorax was unchanged.Conclusions: Precordial ECG changes appear to be a very sensitive indicator of pneumothorax, with very small pneumothorax (<100 cc) consistently being detected by reduction of the QRS complex amplitude. Intraoperative use of precordial ECG leads could result in rapid identification of pneumothorax during laparoscopic surgery. Carbon dioxide pneumothorax shows near 100% resolution in a 2-h period. This supports recommendations of expectant management in asymptomatic patients with CO2 pneumothorax. However, He pneumothorax does not resolve spontaneously quickly and may require aspiration even in asymptomatic patients.



Similar content being viewed by others
References
G Botz JG Brock-Utne (1992) ArticleTitleAre electrocardiogram changes the first sign of impending perioperative pneumothorax?. Anaesthesia 47 1057–1059 Occurrence Handle1:STN:280:ByyC2c3ptVw%3D Occurrence Handle1489031
P Dieter TR Eubanks PE Omelanczuk et al. (2001) ArticleTitleManagement and outcome of complications after laparoscopic antireflux operations. Arch Surg 136 399–404 Occurrence Handle10.1001/archsurg.136.4.399 Occurrence Handle11296109
PJ Girish (2001) ArticleTitleComplications of laparoscopy. Anesth Clin North Am 19 89–105
JL Joris JD Chiche ML Lamy (1995) ArticleTitlePneumothorax during laparoscopic fundoplication: diagnosis and treatment with positive end-expiratory pressure. Anesth Analg 81 993–1000 Occurrence Handle1:STN:280:BymD28fpslY%3D Occurrence Handle7486090
P Kuritzky AL Goldfarb (1976) ArticleTitleUnusual electrocardiographic changes in spontaneous pneumothorax. Chest 70 535–537 Occurrence Handle1:STN:280:CSiD38rjtlw%3D Occurrence Handle975956
MT Makinen A Yli-Hankala M Kansanaho (1995) ArticleTitleEarly detection of CO2 pneumothorax with continuous spirometry during laparoscopic fundoplication. Acta Anaesthesiol Scand 39 411–413 Occurrence Handle1:STN:280:ByqA3MzltFE%3D Occurrence Handle7793226
D Mangar GT Kirchhoff JJ Leal R Laborde E Fu (1994) ArticleTitlePneumothorax during laparoscopic Nissen fundoplication. Can J Anesth 41 854–856 Occurrence Handle1:STN:280:ByqD2c3ps1w%3D
CM Murdock AJ Wolff T Van Geem (2000) ArticleTitleRisk factors for hypercarbia, subcutaneous emphysema, pneumothorax and pneumomediastinum during laparoscopy. Obstet Gynecol 95 704–709
SJ Neuhaus A Gupta DI Watson (2001) ArticleTitleHelium and other alternative gases for laparoscopy. Surg Endosc 15 553–560 Occurrence Handle10.1007/s004640080060 Occurrence Handle1:STN:280:DC%2BD3MrksV2guw%3D%3D Occurrence Handle11591939
DI Watson GG Jamieson R Britten-Jones et al. (1993) ArticleTitlePneumothorax during laparoscopic dissection of the diaphragmatic hiatus. Br J Surg 80 1353–1354 Occurrence Handle1:STN:280:ByuD287kvVI%3D
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ludemann, R., Krysztopik, R., Jamieson, G. et al. Pneumothorax during laparoscopy . Surg Endosc 17, 1985–1989 (2003). https://doi.org/10.1007/s00464-003-8126-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-8126-9