Abstract
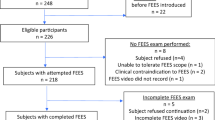
Videofluoroscopic swallow studies (VFSS) provide dynamic assessment of the phases of swallowing under fluoroscopic visualization and allow for identification of abnormalities in the process, such as laryngeal penetration and aspiration. While penetration and aspiration both reflect degrees of swallowing dysfunction, the predictive potential of penetration for subsequent aspiration is not fully elucidated in the pediatric population. As a result, management strategies for penetration vary widely. Some providers may interpret any depth or frequency of penetration as a proxy for aspiration and implement various therapeutic interventions (e.g., modification of liquid viscosity) to eliminate penetration episodes. Some may recommend enteral feeding given the presumed risk of aspiration with penetration, even when aspiration is not identified during the study. In contrast, other providers may advise continued oral feeding without modification even when some degree of laryngeal penetration is identified. We hypothesized that the depth of penetration is associated with the likelihood of aspiration. Identification of predictive factors for aspiration following laryngeal penetration events has significant implications for selection of appropriate interventions. We performed a retrospective cross-sectional analysis of a random sample of 97 patients who underwent VFSS in a single tertiary care center over a 6 month period. Demographic variables including primary diagnosis and comorbidities were analyzed. We examined the association between aspiration and degrees of laryngeal penetration (presence or absence, depth, frequency) across diagnostic categories. Infrequent and shallow penetration events of any type of viscosity were less likely to be associated with aspiration event(s) during the same clinical encounter regardless of diagnosis. In contrast, children with consistent deep penetration of thickened liquids invariably demonstrated aspiration during the same study. Our findings show that shallow, intermittent laryngeal penetration of any viscosity type on VFSS was not consistent with clinical aspiration. These results provide further evidence that penetration-aspiration is not a uniform clinical entity and that nuanced interpretation of videofluoroscopic swallowing findings is necessary to guide appropriate therapeutic interventions.


Similar content being viewed by others

Abbreviations
- VFSS:
-
Videofluoroscopic swallow study
- FEES:
-
Fiberoptic endoscopic evaluations of swallowing
References
Pediatric Feeding and Swallowing [Internet]. [cited 2022 Jan 16]. Available from: https://www.asha.org/practice-portal/clinical-topics/pediatric-feeding-and-swallowing/
Arvedson JC, Lefton-Greif MA. Instrumental assessment of pediatric dysphagia. Semin Speech Lang. 2017;38(2):135–46.
Saad M, Afsah O, Baz H, El-regal ME, Abou-Elsaad T. Clinical and videofluoroscopic evaluation of feeding and swallowing in infants with oropharyngeal dysphagia. Int J Pediatr Otorhinolaryngol. 2021;1:150.
Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia. 2005;20(3):218–25.
Weir KA, McMahon S, Taylor S, Chang AB. Oropharyngeal aspiration and silent aspiration in children. Chest. 2011;140(3):589–97.
Arvedson J, Rogers B, Buck G, Smart P, Msall M. Silent aspiration prominent in children with dysphagia. Int J Pediatr Otorhinolaryngol. 1994;28(2–3):173–81.
Duncan DR, Mitchell PD, Larson K, Rosen RL. Presenting signs and symptoms do not predict aspiration risk in children. J Pediatr. 2018;1(201):141–6.
Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008;19(4):769.
Hartnick CJ, Hartley BEJ, Miller C, Willging JP. Pediatric fiberoptic endoscopic evaluation of swallowing. Ann Otol, Rhinol Laryngol. 2000;109(11):996–9. https://doi.org/10.1177/000348940010901102.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996. https://doi.org/10.1007/BF00417897.
Weir K, McMahon S, Barry L, Ware R, Masters IB, Chang AB. Oropharyngeal aspiration and pneumonia in children. Pediatr Pulmonol. 2007;42(11):1024–31.
Gurberg J, Birnbaum R, Daniel SJ. Laryngeal penetration on videofluoroscopic swallowing study is associated with increased pneumonia in children. Int J Pediatr Otorhinolaryngol. 2015;79(11):1827–30.
Donzelli JJ, Hakel M, Brady SL, Springer T. Spillage, residue, and penetration in healthy adults while swallowing during a meal. Otolaryngol-Head and Neck Surgery. 2016;131(2):P164–P164. https://doi.org/10.1016/j.otohns200406284.
Oliveira DL, Moreira EAM, de Freitas MB, Furkim AM, Clavé P. Pharyngeal residue and aspiration and the relationship with clinical/nutritional status of patients with oropharyngeal dysphagia submitted to videofluoroscopy. J Nutr Health Aging. 2017;21(3):336–41.
Steele CM, Peladeau-Pigeon M, Barrett E, Wolkin TS. The risk of penetration-aspiration related to residue in the pharynx. Am J Speech Lang Pathol. 2020;29(3):1608–17.
Friedman B, Frazier JB. Deep laryngeal penetration as a predictor of aspiration. Dysphagia. 2000 Summer;15(3):153–8.
Dharmarathna I, Miles A, Allen J. Predicting penetration-aspiration through quantitative swallow measures of children: a videofluoroscopic study. European Arch of Oto-Rhino-Laryngol. 2021;278(3):1907–16. https://doi.org/10.1007/s00405-021-06629-4.
McSweeney ME, Kerr J, Amirault J, Mitchell PD, Larson K, Rosen R. Oral feeding reduces hospitalizations compared with gastrostomy feeding in infants and children who aspirate. J Pediatr. 2016;170:79–84.
Stewart A, Burr S. Thickened liquids: do they still have a place in the paediatric dysphagia toolkit? Curr Opin Otolaryngol Head Neck Surg. 2021;29(3):194–9.
Duncan DR, Larson K, Davidson K, May K, Rahbar R, Rosen RL. Feeding interventions are associated with improved outcomes in children with laryngeal penetration. J Pediatr Gastroenterol Nutr. 2019;68(2):218–24.
Friedman B, Frazier JB. Deep laryngeal penetration as a predictor of aspiration. Dysphagia. 2000;15(3):153–8.
Martin-Harris B, Brodsky MB, Michel Y, Castell DP, Schleicher M, Sandidge J, Maxwell, et al. MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405. https://doi.org/10.1007/s00455-008-9185-9.
Gurberg J, Birnbaum R, Daniel SJ. Laryngeal penetration on videofluoroscopic swallowing study is associated with increased pneumonia in children. Int J Pediatr Otorhinolaryngol. 2015;79(11):1827–30.
Coon ER, Srivastava R, Stoddard GJ, Reilly S, Maloney CG, Bratton SL. Infant videofluoroscopic swallow study testing, swallowing interventions, and future acute respiratory illness. Hosp Pediatr. 2016;6(12):707–13.
Adlakha V, Ramos L, Smith A, Tsistinas O, Tanner-Smith E, Merrow J, et al. Risk of aspiration pneumonia in paediatric patients with dysphagia who were found to have laryngeal penetration on the instrumental swallow evaluation: a systematic review protocol. BMJ Open. 2021;11(8):e048422.
Duncan DR, Larson K, Davidson K, May K, Rahbar R, Rosen RL. Feeding interventions are associated with improved outcomes in children with laryngeal penetration. J Pediatr Gastroenterol Nutr. 2019;68(2):218–24.
Lee JW, Randall DR, Evangelista LM, Kuhn MA, Belafsky PC. Subjective assessment of videofluoroscopic swallow studies. Otolaryngology - Head and Neck Surgery (United States). 2017;156(5):901–5.
Funding
This project was not supported by any external grants or funds. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller, A.L., Miller, C.K., Fei, L. et al. Predictive Value of Laryngeal Penetration to Aspiration in a Cohort of Pediatric Patients. Dysphagia 39, 33–42 (2024). https://doi.org/10.1007/s00455-023-10589-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10589-8