Abstract
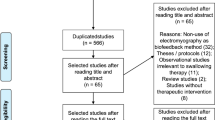
Despite rapid growth in the number of treatments to rehabilitate dysphagia, studies often demonstrate mixed results with non-significant changes to functional outcomes. Given that power analyses are infrequently reported in dysphagia research, it remains unclear whether studies are adequately powered to detect a range of treatment effects. Therefore, this review sought to examine the current landscape of statistical power in swallowing rehabilitation research. Databases were searched for swallowing treatments using instrumental evaluations of swallowing and the penetration–aspiration scale as an outcome. Sensitivity power analyses based on each study’s statistical test and sample size were performed to determine the minimum effect size detectable with 80% power. Eighty-nine studies with 94 treatment comparisons were included. Sixty-seven percent of treatment comparisons were unable to detect effects smaller than d = 0.80. The smallest detectable effect size was d = 0.29 for electrical stimulation, d = 0.49 for postural maneuvers, d = 0.52 for non-invasive brain stimulation, d = 0.61 for combined treatments, d = 0.63 for respiratory-based interventions, d = 0.70 for lingual strengthening, and d = 0.79 for oral sensory stimulation. Dysphagia treatments examining changes in penetration–aspiration scale scores were generally powered to reliably detect larger effect sizes and not smaller (but potentially clinically meaningful) effects. These findings suggest that non-significant results may be related to low statistical power, highlighting the need for collaborative, well-powered intervention studies that can detect smaller, clinically meaningful changes in swallowing function. To facilitate implementation, a tutorial on simulation-based power analyses for ordinal outcomes is provided (https://osf.io/e6usd/).


Similar content being viewed by others
Data Availability and Supplemental Power Analysis Tutorial
The data analysis script and a supplemental tutorial on performing simulation-based power analyses with ordinal outcomes are available on the Open Science Framework at the following url: https://osf.io/65atf/.
References
Mancopes R, Smaoui S, Steele CM. Effects of expiratory muscle strength training on videofluoroscopic measures of swallowing: a systematic review. Am J Speech Lang Pathol. 2020;30:1–22.
Langmore SE, Pisegna JM. Efficacy of exercises to rehabilitate dysphagia: a critique of the literature. Int J Speech Lang Pathol. 2015;17(3):222–9.
Bothe AK, Richardson JD. Statistical, practical, clinical, and personal significance: definitions and applications in speech-language pathology. Am J Speech Lang Pathol. 2011;20(3):233–42.
Hedström J, Tuomi L, Andersson M, Dotevall H, Osbeck H, Finizia C. Within-bolus variability of the penetration-aspiration scale across two subsequent swallows in patients with head and neck cancer. Dysphagia. 2017;32(5):683–90.
Molfenter SM, Steele CM. Physiological variability in the deglutition literature: hyoid and laryngeal kinematics. Dysphagia. 2011;26(1):67–74.
Molfenter SM, Steele CM. Temporal variability in the deglutition literature. Dysphagia. 2012;27(2):162–77.
Ahadi S, Diener E. Multiple determinants and effect size. J Pers Soc Psychol. 1989;56(3):398–406.
Neyman J, Pearson ES. The testing of statistical hypotheses in relation to probabilities a priori. Math Proc Camb Philos Soc. 1933;29(4):492–510.
Bacchetti P. Current sample size conventions: flaws, harms, and alternatives. BMC Med. 2010;8(1):17.
Neyman J. Frequentist probability and frequentist statistics. Synthese. 1977;36(1):97–131.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: L. Erlbaum Associates; 1988.
Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14(5):365–76.
Szucs D, Ioannidis JPA. Empirical assessment of published effect sizes and power in the recent cognitive neuroscience and psychology literature. PLoS Biol. 2017;15(3):1–18.
Yarkoni T. Big correlations in little studies: inflated fMRI correlations reflect low statistical power—commentary on Vul et al. (2009). Perspect Psychol Sci. 2009;4(3):294–8.
Gelman A, Carlin J. Beyond power calculations: assessing type S (sign) and type M (magnitude) errors. Perspect Psychol Sci. 2014;9(6):641–51.
Ioannidis JPA. Why most published research findings are false. PLoS Med. 2005;2(8):696–701.
Ioannidis JPA, Tarone R, McLaughlin JK. The false-positive to false-negative ratio in epidemiologic studies. Epidemiology. 2011;22(4):450–6.
Ioannidis JPA. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640–8.
Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan A-W, Cronin E, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS ONE. 2008;3(8):1–31.
Borders JC, Brates D. Use of the penetration-aspiration scale in dysphagia research: a systematic review. Dysphagia. 2019;35(4):583–97.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–9.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.R-project.org/.
Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Caldwell AR, Lakens D, Parlett-Pelleriti CM. Power analysis with superpower. 2019. https://aaroncaldwell.us/SuperpowerBook/. Accessed 20 Nov 2020.
Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013. https://doi.org/10.3389/fpsyg.2013.00863.
Baijens LWJ, Speyer R, Passos VL, Pilz W, van der Kruis J, Haarmans S, et al. Surface electrical stimulation in dysphagic parkinson patients: a randomized clinical trial: electrical stimulation for dysphagia in Parkinson. Laryngoscope. 2013;123(11):E38-44.
Rogus-Pulia N, Rusche N, Hind JA, Zielinski J, Gangnon R, Safdar N, et al. Effects of device-facilitated isometric progressive resistance oropharyngeal therapy on swallowing and health-related outcomes in older adults with dysphagia. J Am Geriatr Soc. 2016;64(2):417–24.
Wall LR, Ward EC, Cartmill B, Hill AJ, Isenring E, Byrnes J, et al. Prophylactic swallowing therapy for patients with head and neck cancer: a three-arm randomized parallel-group trial. Head Neck. 2020;42(5):873–85.
Messing BP. Prophylactic swallow therapy for patients with head and neck cancer undergoing chemoradiotherapy: a randomized trial. Dysphagia. 2017;32(4):487–500.
Van Daele DJ, Langmore SE, Krisciunas GP, Lazarus CL, Pauloski BR, McCulloch TM, et al. The impact of time after radiation treatment on dysphagia in patients with head and neck cancer enrolled in a swallowing therapy program. Head Neck. 2019;41(3):606–14.
Guillén-Solà A, Messagi Sartor M, Bofill Soler N, Duarte E, Barrera MC, Marco E. Respiratory muscle strength training and neuromuscular electrical stimulation in subacute dysphagic stroke patients: a randomized controlled trial. Clin Rehabil. 2017;31(6):761–71.
Lim KB, Lee HJ, Yoo J, Kwon YG. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Ann Rehabil Med. 2014;38(5):592–602.
Terré R, Mearin F. A randomized controlled study of neuromuscular electrical stimulation in oropharyngeal dysphagia secondary to acquired brain injury. Eur J Neurol. 2015;22(4):687-e44.
Simonelli M, Ruoppolo G, Iosa M, Morone G, Fusco A, Grasso MG, et al. A stimulus for eating. The use of neuromuscular transcutaneous electrical stimulation in patients affected by severe dysphagia after subacute stroke: a pilot randomized controlled trial. NeuroRehabilitation. 2019;44:103–310.
Lee HY, Hong JS, Lee KC, Shin YK, Cho SR. Changes in hyolaryngeal movement and swallowing function after neuromuscular electrical stimulation in patients with dysphagia. Ann Rehabil Med. 2015;39(2):199–209.
Sun S-F, Hsu C-W, Lin H-S, Sun H-P, Chang P-H, Hsieh W-L, et al. Combined neuromuscular electrical stimulation (NMES) with fiberoptic endoscopic evaluation of swallowing (FEES) and traditional swallowing rehabilitation in the treatment of stroke-related dysphagia. Dysphagia. 2013;28(4):557–66.
Ko KR, Park HJ, Hyun JK, Seo IH, Kim TU. Effect of laryngopharyngeal neuromuscular electrical stimulation on dysphonia accompanied by dysphagia in post-stroke and traumatic brain injury patients: a pilot study. Ann Rehabil Med. 2016;40(4):600–10.
Park J-S, Hwang N-K, Kim H-H, Lee G, Jung Y-J. Effect of neuromuscular electrical stimulation combined with effortful swallowing using electromyographic biofeedback on oropharyngeal swallowing function in stroke patients with dysphagia: a pilot study. Medicine. 2019;98(44):1–6.
Rofes L, Arreola V, López I, Martin A, Sebastián M, Ciurana A, et al. Effect of surface sensory and motor electrical stimulation on chronic poststroke oropharyngeal dysfunction. Neurogastroenterol Motil. 2013;25(11):888–96.
Lin PH, Hsiao TY, Chang YC, Ting LL, Chen WS, Chen SC, et al. Effects of functional electrical stimulation on dysphagia caused by radiation therapy in patients with nasopharyngeal carcinoma. Support Care Cancer. 2011;19(1):91–9.
Jeon YH, Cho KH, Park SJ. Effects of neuromuscular electrical stimulation (NMES) plus upper cervical spine mobilization on forward head posture and swallowing function in stroke patients with dysphagia. Brain Sci. 2020;10(8):1–10.
Park JS, Oh DH, Hwang NK, Lee JH. Effects of neuromuscular electrical stimulation combined with effortful swallowing on post-stroke oropharyngeal dysphagia: a randomised controlled trial. J Oral Rehabil. 2016;43(6):426–34.
Lee KW, Kim SB, Lee JH, Lee SJ, Park JG, Jang KW. Effects of neuromuscular electrical stimulation for masseter muscle on oral dysfunction after stroke. Ann Rehabil Med. 2019;43(1):11–8.
Park JS, Oh DH, Hwang NK, Lee JH. Effects of neuromuscular electrical stimulation in patients with Parkinson’s disease and dysphagia: a randomized, single-blind, placebo-controlled trial. NeuroRehabilitation. 2018;42(4):457–63.
Mituuti CT, Arone MMAS, Rosa RR, Berretin-Felix G. Effects of sensory neuromuscular electrical stimulation on swallowing in the elderly affected by stroke. Top Geriatr Rehabil. 2018;34(1):71–81.
Langmore SE, McCulloch TM, Krisciunas GP, Lazarus CL, Van Daele DJ, Pauloski BR, et al. Efficacy of electrical stimulation and exercise for dysphagia in patients with head and neck cancer: a randomized clinical trial. Head Neck. 2015;38:1221–31.
Park JW, Kim Y, Oh JC, Lee HJ. Effortful swallowing training combined with electrical stimulation in post-stroke dysphagia: a randomized controlled study. Dysphagia. 2012;27(4):521–7.
Huang KL, Liu TY, Huang YC, Leong CP, Lin WC, Pong YP. Functional outcome in acute stroke patients with oropharyngeal dysphagia after swallowing therapy. J Stroke Cerebrovasc Dis. 2014;23(10):2547–53.
Bhatt AD, Goodwin N, Cash E, Bhatt G, Silverman CL, Spanos WJ, et al. Impact of transcutaneous neuromuscular electrical stimulation on dysphagia in patients with head and neck cancer treated with definitive chemoradiation. Head Neck. 2015;37(7):1051–6.
Lim KB, Lee HJ, Lim SS, Choi YI. Neuromuscular electrical and thermal-tactile stimulation for dysphagia caused by stroke: a randomized controlled trial. J Rehabil Med. 2009;41(3):174–8.
Martindale N, Stephenson J, Pownall S. Neuromuscular electrical stimulation plus rehabilitative exercise as a treatment for dysphagia in stroke and non-stroke patients in an NHS setting: feasibility and outcomes. Geriatrics. 2019;4(4):53.
Gallas S, Marie JP, Leroi AM, Verin E. Sensory transcutaneous electrical stimulation improves post-stroke dysphagic patients. Dysphagia. 2010;25(4):291–7.
Oh D-H, Park J-S, Kim H-J, Chang M-Y, Hwang N-K. The effect of neuromuscular electrical stimulation with different electrode positions on swallowing in stroke patients with oropharyngeal dysphagia: a randomized trial. J Back Musculoskelet Rehabil. 2019;33(4):637–44.
Bogaardt H, van Dam D, Wever NM, Bruggeman CE, Koops J, Fokkens WJ. Use of neuromuscular electrostimulation in the treatment of dysphagia in patients with multiple sclerosis. Ann Otol Rhinol Laryngol. 2009;118(4):241–6.
Arreola V, Ortega O, Álvarez-Berdugo D, Rofes L, Tomsen N, Cabib C, et al. Effect of transcutaneous electrical stimulation in chronic poststroke patients with oropharyngeal dysphagia: 1-year results of a randomized controlled trial. Neurorehabil Neural Repair. 2021;17:154596832110231.
Bath PM, Scutt P, Love J, Clavé P, Cohen D, Dziewas R, et al. Pharyngeal electrical stimulation for treatment of dysphagia in subacute stroke: a randomized controlled trial. Stroke. 2016;47(6):1562–70.
Everton LF, Benfield JK, Michou E, Hamdy S, Bath PM. Effects of pharyngeal electrical stimulation on swallow timings, clearance and safety in post-stroke dysphagia: analysis from the swallowing treatment using electrical pharyngeal stimulation (STEPS) trial. Stroke Res Treat. 2021;2021:1–8.
Hägglund P, Hägg M, Levring Jäghagen E, Larsson B, Wester P. Oral neuromuscular training in patients with dysphagia after stroke: a prospective, randomized, open-label study with blinded evaluators. BMC Neurol. 2020;20(1):405.
Jayasekeran V, Singh S, Tyrrell P, Michou E, Jefferson S, Mistry S, et al. Adjunctive functional pharyngeal electrical stimulation reverses swallowing disability after brain lesions. Gastroenterology. 2010;138(5):1737–46.
Lee SY, Park D, Jang J, Jang EG, Lee JC, Park Y, et al. Compensatory effects of sequential 4-channel neuromuscular electrical stimulation for the treatment of acute, subacute, and chronic dysphagia in a prospective, double-blinded randomized clinical trial. Neurorehabil Neural Repair. 2021. https://doi.org/10.1177/15459683211029891.
Ludlow CL, Humbert I, Saxon K, Poletto C, Sonies B, Crujido L. Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal dysphagia. Dysphagia. 2007;22(1):1–10.
Restivo DA, Casabona A, Centonze D, Marchese-Ragona R, Maimone D, Pavone A. Pharyngeal electrical stimulation for dysphagia associated with multiple sclerosis: a pilot study. Brain Stimul. 2013;6(3):418–23.
Seo K-H, Jang J, Jang EG, Park Y, Lee SY, Kim BR, et al. Clinical effectiveness of the sequential 4-channel NMES compared with that of the conventional 2-channel NMES for the treatment of dysphagia in a prospective double-blind randomized controlled study. J NeuroEng Rehabil. 2021;18(1):90.
Miller S, Diers D, Jungheim M, Schnittger C, Stürenburg HJ, Ptok M. Studying effects of neuromuscular electrostimulation therapy in patients with dysphagia: which pitfalls may occur? A translational phase I study. Ger Med Sci. 2021;19:Doc07.
Ortega O, Rofes L, Martin A, Arreola V, López I, Clavé P. A comparative study between two sensory stimulation strategies after two weeks treatment on older patients with oropharyngeal dysphagia. Dysphagia. 2016;31(5):706–16.
Bath PM, Woodhouse LJ, Suntrup-Krueger S, Likar R, Koestenberger M, Warusevitane A, et al. Pharyngeal electrical stimulation for neurogenic dysphagia following stroke, traumatic brain injury or other causes: main results from the PHADER cohort study. EClinicalMedicine. 2020;28:100608.
Michou E, Mistry S, Jefferson S, Tyrrell P, Hamdy S. Characterizing the mechanisms of central and peripheral forms of neurostimulation in chronic dysphagic stroke patients. Brain Stimul. 2014;7(1):66–73.
Vasant DH, Michou E, O’Leary N, Vail A, Mistry S, Hamdy S. Pharyngeal electrical stimulation in dysphagia poststroke. Neurorehabil Neural Repair. 2016;30(9):866–75.
Verin E, Maltete D, Ouahchi Y, Marie J-P, Hannequin D, Massardier EG, et al. Submental sensitive transcutaneous electrical stimulation (SSTES) at home in neurogenic oropharyngeal dysphagia: a pilot study. Ann Phys Rehabil Med. 2011;54(6):366–75.
Park J, Kim H, Park T, Yeo J, Hong H, Oh J. A pilot study of the effects of high-frequency repetitive transcranial magnetic stimulation on dysphagia in the elderly. Neurogastroenterol Motil. 2019;31(5):1–6.
Restivo DA, Alfonsi E, Casabona A, Hamdy S, Tassorelli C, Panebianco M, et al. A pilot study on the efficacy of transcranial direct current stimulation applied to the pharyngeal motor cortex for dysphagia associated with brainstem involvement in multiple sclerosis. Clin Neurophysiol. 2019;130(6):1017–24.
Lee JH, Kim SB, Lee KW, Lee SJ, Lee JU. Effect of repetitive transcranial magnetic stimulation according to the stimulation site in stroke patients with dysphagia. Ann Rehabil Med. 2015;39(3):432–9.
Kim L, Chun MH, Kim BR, Lee SJ. Effect of repetitive transcranial magnetic stimulation on patients with brain injury and dysphagia. Ann Rehabil Med. 2011;35(6):765–71.
Park E, Kim MS, Chang WH, Oh SM, Kim YK, Lee A, et al. Effects of bilateral repetitive transcranial magnetic stimulation on post-stroke dysphagia. Brain Stimul. 2017;10(1):75–82.
Ünlüer NÖ, Temuçin ÇM, Demir N, Serel Arslan S, Karaduman AA. Effects of low-frequency repetitive transcranial magnetic stimulation on swallowing function and quality of life of post-stroke patients. Dysphagia. 2019;34(3):360–71.
Verin E, Leroi AM. Poststroke dysphagia rehabilitation by repetitive transcranial magnetic stimulation: a noncontrolled pilot study. Dysphagia. 2009;24(2):204–10.
Michou E, Mistry S, Jefferson S, Singh S, Rothwell J, Hamdy S. Targeting unlesioned pharyngeal motor cortex improves swallowing in healthy individuals and after dysphagic stroke. Gastroenterology. 2012;142(1):29–38.
Park JW, Oh JC, Lee JW, Yeo JS, Ryu KH. The effect of 5Hz high-frequency rTMS over contralesional pharyngeal motor cortex in post-stroke oropharyngeal dysphagia: a randomized controlled study. Neurogastroenterol Motil. 2013;25(4):324–31.
Khedr EM, Mohamed KO, Soliman RK, Hassan AMM, Rothwell JC. The effect of high-frequency repetitive transcranial magnetic stimulation on advancing parkinson’s disease with dysphagia: double blind randomized clinical trial. Neurorehabil Neural Repair. 2019;33(6):442–52.
Lin WS, Chou CL, Chang MH, Chung YM, Lin FG, Tsai PY. Vagus nerve magnetic modulation facilitates dysphagia recovery in patients with stroke involving the brainstem—a proof of concept study. Brain Stimul. 2018;11(2):264–70.
Zhong L, Rao J, Wang J, Li F, Peng Y, Liu H, et al. Repetitive transcranial magnetic stimulation at different sites for dysphagia after stroke: a randomized, observer-blind clinical trial. Front Neurol. 2021;12:625683.
Troche MS, Okun MS, Rosenbek JC, Musson N, Fernandez HH, Rodriguez R, et al. Aspiration and swallowing in Parkinson disease and rehabilitation with EMST: a randomized trial. Neurology. 2010;75(21):1912–9.
Park JS, Oh DH, Chang MY, Kim KM. Effects of expiratory muscle strength training on oropharyngeal dysphagia in subacute stroke patients: a randomised controlled trial. J Oral Rehabil. 2016;43(5):364–72.
Moon JH, Jung J-H, Won YS, Cho H-Y, Cho K. Effects of expiratory muscle strength training on swallowing function in acute stroke patients with dysphagia. J Phys Ther Sci. 2017;29:609–12.
Eom MJ, Chang MY, Oh DH, Kim HD, Han NM, Park JS. Effects of resistance expiratory muscle strength training in elderly patients with dysphagic stroke. NeuroRehabilitation. 2017;41(4):747–52.
Hutcheson KA, Barrow MP, Plowman EK, Lai SY, Fuller CD, Barringer DA, et al. Expiratory muscle strength training for radiation-associated aspiration after head and neck cancer: a case series. Laryngoscope. 2017;128(5):1044–51.
Pitts T, Bolser D, Rosenbek J, Troche MS, Okun MS, Sapienza C. Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease. Chest. 2009;135(5):1301–8.
Plowman EK, Tabor-Gray L, Rosado KM, Vasilopoulos T, Robison R, Chapin JL, et al. Impact of expiratory strength training in amyotrophic lateral sclerosis: results of a randomized, sham-controlled trial. Muscle Nerve. 2019;59(1):40–6.
Plowman EK, Watts SA, Tabor L, Robison R, Gaziano J, Domer AS, et al. Impact of expiratory strength training in amyotrophic lateral sclerosis: expiratory training in ALS. Muscle Nerve. 2016;54(1):48–53.
Hegland KW. Rehabilitation of swallowing and cough functions following stroke: an expiratory muscle strength training trial. Arch Phys Med Rehabil. 2016;97(8):1345–51.
Mohannak N, Pattison G, Radich B, Hird K, Godecke E, Mastaglia F, et al. Exploring the efficacy of the expiratory muscle strength trainer to improve swallowing in inclusion body myositis: a pilot study. Neuromuscul Disord. 2020;30(4):294–300.
Arnold RJ, Bausek N. Effect of respiratory muscle training on dysphagia in stroke patients—a retrospective pilot study. Laryngosc Investig Otolaryngol. 2020;5(6):1050–5.
Jang K, Lee S, Kim S, Lee K, Lee J, Park J. Effects of mechanical inspiration and expiration exercise on velopharyngeal incompetence in subacute stroke patients. J Rehabil Med. 2019;51(2):97–102.
Martin-Harris B, McFarland D, Hill EG, Strange CB, Focht KL, Wan Z, et al. Respiratory-swallow training in patients with head and neck cancer. Arch Phys Med Rehabil. 2015;96(5):885–93.
Choi J-B, Shim S-H, Yang J-E, Kim H-D, Lee D-H, Park J-S. Effects of Shaker exercise in stroke survivors with oropharyngeal dysphagia. NeuroRehabilitation. 2017;41(4):753–7.
Gao J, Zhang H-J. Effects of chin tuck against resistance exercise versus Shaker exercise on dysphagia and psychological state after cerebral infarction. Eur J Phys Rehabil Med. 2017;53(3):426–32.
Kim H, Park J. Efficacy of modified chin tuck against resistance exercise using hand-free device for dysphagia in stroke survivors: a randomised controlled trial. J Oral Rehabil. 2019;46(11):1042–6.
Mano T, Katsuno M, Banno H, Suzuki K, Suga N, Hashizume A, et al. Head lift exercise improves swallowing dysfunction in spinal and bulbar muscular atrophy. Eur Neurol. 2015;74(5–6):251–8.
Park JS, Hwang NK, Oh DH, Chang MY. Effect of head lift exercise on kinematic motion of the hyolaryngeal complex and aspiration in patients with dysphagic stroke. J Oral Rehabil. 2017;44(5):385–91.
Park JS, An DH, Oh DH, Chang MY. Effect of chin tuck against resistance exercise on patients with dysphagia following stroke: a randomized pilot study. NeuroRehabilitation. 2018;42(2):191–7.
Park J, Lee G, Jung Y. Effects of game-based chin tuck against resistance exercise vs head-lift exercise in patients with dysphagia after stroke: an assessor-blind, randomized controlled trial. J Rehabil Med. 2019;51(10):749–54.
Park J-S, An D-H, Kam K-Y, Yoon T, Kim T, Chang M-Y. Effects of resistive jaw opening exercise in stroke patients with dysphagia: a double-blind, randomized controlled study. BMR. 2020;33(3):507–13.
Ploumis A, Papadopoulou SL, Theodorou SJ, Exarchakos G, Givissis P, Beris A. Cervical isometric exercises improve dysphagia and cervical spine malalignment following stroke with hemiparesis: a randomized controlled trial. Eur J Phys Rehabil Med. 2019;54(6):845–52.
Jakobsen D, Poulsen I, Schultheiss C, Riberholt CG, Curtis DJ, Petersen TH, et al. The effect of intensified nonverbal facilitation of swallowing on dysphagia after severe acquired brain injury: a randomised controlled pilot study. NRE. 2019;45(4):525–36.
Power ML, Fraser CH, Hobson A, Singh S, Tyrrell P, Nicholson DA, et al. Evaluating oral stimulation as a treatment for dysphagia after stroke. Dysphagia. 2006;21(1):49–55.
Rosenbek JC, Robbins J, Willford WO, Kirk G, Schiltz A, Sowell TW, et al. Comparing treatment intensities of tactile-thermal application. Dysphagia. 1998;13(1):1–9.
Tomsen N, Ortega O, Rofes L, Arreola V, Martin A, Mundet L, et al. Acute and subacute effects of oropharyngeal sensory stimulation with TRPV1 agonists in older patients with oropharyngeal dysphagia: a biomechanical and neurophysiological randomized pilot study. Ther Adv Gastroenterol. 2019. https://doi.org/10.1177/1756284819842043.
Steele CM, Bayley MT, Peladeau-Pigeon M, Nagy A, Namasivayam AM, Stokely SL, et al. A randomized trial comparing two tongue-pressure resistance training protocols for post-stroke dysphagia. Dysphagia. 2016;31:452–61.
Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150–8.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483–9.
Namiki C, Hara K, Tohara H, Kobayashi K, Chantaramanee A, Nakagawa K, et al. Tongue-pressure resistance training improves tongue and suprahyoid muscle functions simultaneously. CIA. 2019;14:601–8.
Kim HD, Choi JB, Yoo SJ, Chang MY, Lee SW, Park JS. Tongue-to-palate resistance training improves tongue strength and oropharyngeal swallowing function in subacute stroke survivors with dysphagia. J Oral Rehabil. 2017;44(1):59–64.
Balou M, Herzberg EG, Kamelhar D, Molfenter SM. An intensive swallowing exercise protocol for improving swallowing physiology in older adults with radiographically confirmed dysphagia. CIA. 2019;14:283–8.
Hsiang C-C, Chen AW-G, Chen C-H, Chen M-K. Early postoperative oral exercise improves swallowing function among patients with oral cavity cancer: a randomized controlled trial. Ear Nose Throat J. 2019;98(6):E73–80.
Kraaijenga SAC, van der Molen L, Stuiver MM, Takes RP, Al-Mamgani A, van den Brekel MWM, et al. Efficacy of a novel swallowing exercise program for chronic dysphagia in long-term head and neck cancer survivors. Head Neck. 2017;39(10):1943–61.
Tarameshlu M. The effect of traditional dysphagia therapy on the swallowing function in patients with multiple sclerosis: a pilot double-blinded randomized controlled trial. J Bodyw Mov Ther. 2019;23(1):171–6.
van der Molen L, van Rossum MA, Burkhead LM, Smeele LE, Rasch CR, Hilgers FJ. A randomized preventive rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance, and short-term effects. Dysphagia. 2011;26(2):155–70.
van der Molen L, van Rossum MA, Rasch CRN, Smeele LE, Hilgers FJM. Two-year results of a prospective preventive swallowing rehabilitation trial in patients treated with chemoradiation for advanced head and neck cancer. Eur Arch Otorhinolaryngol. 2014;271(5):1257–70.
Furuie H, Hamamoto T, Chikuie N, Kono T, Taruya T, Ishino T, et al. Evaluation of role of prophylactic swallowing rehabilitation in chemoradiotherapy for advanced head and neck cancer using novel software analysis of videofluorography images. Hiroshima J Med Sci. 2019;68(2–3):27–34.
Boukrina O, Kucukboyaci NE, Dobryakova E. Considerations of power and sample size in rehabilitation research. Int J Psychophysiol. 2020;154:6–14.
Knottnerus JA, Bouter LM. The ethics of sample size: two-sided testing and one-sided thinking. J Clin Epidemiol. 2001;54:109–10.
Lakens D. Performing high-powered studies efficiently with sequential analyses: sequential analyses. Eur J Soc Psychol. 2014;44(7):701–10.
Lakens D. Will knowledge about more efficient study designs increase the willingness to pre-register? https://osf.io/svzyc. Accessed Mar 2017.
Brysbaert M, Stevens M. Power analysis and effect size in mixed effects models: a tutorial. J Cogn. 2018;1(1):9.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med. 2020. https://doi.org/10.1056/nejmoa2034577.
Zhang JJ, Blumenthal GM, He K, Tang S, Cortazar P, Sridhara R. Overestimation of the effect size in group sequential trials. Clin Cancer Res. 2012;18(18):4872–6.
Project J. The jamovi project. 2020. (jamovi). https://www.jamovi.org.
Johnson PCD, Barry SJE, Ferguson HM, Mu P. Power analysis for generalized linear mixed models in ecology and evolution. Methods Ecol Evol. 2014;6:133–42.
Quintana DS. A synthetic dataset primer for the biobehavioural sciences to promote reproducibility and hypothesis generation. Elife. 2020;9:1–12.
Quintana DS. Most oxytocin administration studies are statistically underpowered to reliably detect (or reject) a wide range of effect sizes. Compr Psychoneuroendocrinol. 2020;4:1–4.
Funding
N/A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borders, J.C., Grande, A.A. & Troche, M.S. Statistical Power and Swallowing Rehabilitation Research: Current Landscape and Next Steps. Dysphagia 37, 1673–1688 (2022). https://doi.org/10.1007/s00455-022-10428-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10428-2