Abstract
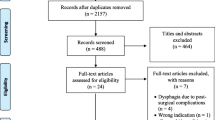
Resistant arterial hypertension (RAH) is strongly associated with obstructive sleep apnea (OSA). Individuals with OSA may have subclinical swallow impairment, diagnosed by instrumental assessments, such as videofluoroscopy and fiberoptic endoscopic evaluation of swallowing (FEES). However, few studies have evaluated this population and included a control group of individuals without OSA. To evaluate, through FEES, the swallowing characteristics of resistant hypertensive patients with and without OSA and to investigate the association between the signs of swallow impairment and OSA. This was an observational study in which individuals with RAH underwent baseline polysomnography and were diagnosed with and without OSA. All participants underwent an initial assessment with the collection of demographic characteristics and FEES. Individuals were divided into 2 groups based on the presence or absence of OSA. Seventy-nine resistant hypertensive patients were evaluated: 60 with OSA (19 with mild OSA, 21 with moderate OSA, and 20 with severe OSA) and 19 without OSA. The most prevalent swallowing differences between groups with and without OSA were piecemeal deglutition, in 61.7% and 31.6%, respectively (p = 0.022); spillage, in 58.3% and 21.1% (p = 0.005); penetration/aspiration, in 55% and 47.4% (p = 0.561); and pharyngeal residue, in 51.5% and 26.3% (p = 0.053). The prevalence of swallow impairment among the participants in this study was 58.3% and 47.4% in the groups with OSA and without OSA, respectively (p = 0.402). This study shows a high prevalence of swallow impairment both in hypertensive patients with OSA and without OSA. The characteristics of swallowing associated with hypertensive patients with OSA are spillage, piecemeal deglutition, and the onset of the pharyngeal phase in the hypopharynx.

Similar content being viewed by others
References
Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5):e53–90. https://doi.org/10.1161/HYP.0000000000000084.
Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57(6):1076–80. https://doi.org/10.1161/HYPERTENSIONAHA.111.170308.
Muxfeldt ES, Margallo VS, Guimarães GM, Salles GF. Prevalence and associated factors of obstructive sleep apnea in patients with resistant hypertension. Am J Hypertens. 2014;27(8):1069–78. https://doi.org/10.1093/ajh/hpu023.
Sapiña-Beltrán E, Torres G, Benitez I, Fortuna-Gutiérrez AM, Márquez PP, Masa JF, et al. Prevalence, characteristics, and association of obstructive sleep apnea with blood pressure control in patients with resistant hypertension. Ann Am Thorac Soc. 2019;16(11):1414–21. https://doi.org/10.1513/AnnalsATS.201901-053OC.
Parati G, Lombardi C, Hedner J, Bonsignore MR, Grote L, Tkacova R, et al. Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (COoperation in Scientific and Technological research) ACTION B26 on obstructive sleep apnea. J Hypertens. 2012;30(4):633–46. https://doi.org/10.1097/HJH.0b013e328350e53b.
Shah F, Franklin KA, Holmlund T, Jäghagen EL, Berggren D, Forsgren S, Stål P. Desmin and dystrophin abnormalities in upper airway muscles of snorers and patients with sleep apnea. Respir Res. 2019;20(1):31. https://doi.org/10.1186/s12931-019-0999-9.
Oliveira LAMDP, Fontes LHDS, Cahali MB. Swallowing and pharyngo-esophageal manometry in obstructive sleep apnea. Braz J Otorhinolaryngol. 2015;81(3):294–300. https://doi.org/10.1016/j.bjorl.2015.03.006.
Levring Jäghagen E, Franklin K, Isberg A. Snoring, sleep apnoea and swallowing dysfunction: a videoradiographic study. Dentomaxillofacial Radiology. 2003;32(5):311–6. https://doi.org/10.1259/dmfr/29209140.
Valarelli L, Corradi A, Grechi T, Eckeli A, Aragon D, Küpper D, et al. Cephalometric, muscular, and swallowing changes in patients with OSAS. J Oral Rehabil. 2018;45(9):692–701. https://doi.org/10.1111/joor.12666.
Campanholo MDAT, de Azevedo Caparroz F, Stefanini R, Haddad L, Bittencourt LRA, Tufik S, Haddad FLM. Dysphagia in patients with moderate and severe obstructive sleep apnea. Brazilian Journal of Otorhinolaryngology. 2019;S1808–8694(19):30137–45. https://doi.org/10.1016/j.bjorl.2019.10.004.
Caparroz FA, Campanholo MDAT, Sguillar DA, Haddad L, Park SW, Bittencourt L, Tufik S, Haddad FLM. A pilot study on the efficacy of continuous positive airway pressure on the manifestations of dysphagia in patients with obstructive sleep apnea. Dysphagia. 2019;34(3):333–40. https://doi.org/10.1007/s00455-018-9944-1.
Schindler A, Mozzanica F, Sonzini G, Plebani D, Urbani E, Pecis M, Montano N. Oropharyngeal dysphagia in patients with obstructive sleep apnea syndrome. Dysphagia. 2014;29(1):44–51. https://doi.org/10.1007/s00455-013-9474-9.
Valbuza JS, de Oliveira MM, Zancanella E, Conti CF, Prado LBF, Carvalho LB, do Prado GF. Swallowing dysfunction related to obstructive sleep apnea: a nasal fibroscopy pilot study. Sleep Breath. 2011;15(2):209–13. https://doi.org/10.1007/s11325-010-0474-9.
Yin T, Jardine M, Miles A, Allen J. What is a normal pharynx? A videofluoroscopic study of anatomy in older adults. Eur Arch Otorhinolaryngol. 2018;275(9):2317–23. https://doi.org/10.1007/s00405-018-5057-6.
Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope. 2003;113(8):1386–93. https://doi.org/10.1097/00005537-200308000-00023.
Matsuo K, Kawase S, Wakimoto N, Iwatani K, Masuda Y, Ogasawara T. Effect of viscosity on food transport and swallow initiation during eating of two-phase food in normal young adults: a pilot study. Dysphagia. 2013;28(1):63–8. https://doi.org/10.1007/s00455-012-9413-1.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration aspiration scale. Dysphagia. 1996;11(2):93–8. https://doi.org/10.1007/BF00417897.
Neubauer PD, Rademaker AW, Leder SB. The Yale pharyngeal residue severity rating scale: an anatomically defined and iamge-based tool. Dysphagia. 2015;30(5):521–8. https://doi.org/10.1007/s00455-015-9631-4.
O’Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome and severity scale. Dysphagia. 1999;14(3):139–45. https://doi.org/10.1007/PL00009595.
Wang CM, Chen JY, Chuang CC, Tseng WC, Wong AM, Pei YC. Aging-related changes in swallowing, and in the coordination of swallowing and respiration determined by novel non-invasive measurement techniques. Geriatr Gerontol Int. 2015;15(6):736–44. https://doi.org/10.1111/ggi.12343.
Teramoto S, Ishii T, Matsuse T. Relationship between swallowing function and gas exchange during day and night in patients with obstructive sleep apnea syndrome. Dysphagia. 2001;16(4):249–53. https://doi.org/10.1007/s00455-001-0083-7.
Yüksel A, Kulan CA, Bilgin RR, Ünsal YO, Yurtman N, Akçiçek F, Uluer H. Examination of the relationship of asymptomatic swallowing disorder prevalence with hypertension, diabetes and obesity in elderly population. J Geriatr Med Gerontol. 2019;5:071. https://doi.org/10.23937/2469-5858/1510071.
Steele CM, Grace-Martin K. Reflections on clinical and statistical use of the penetration-aspiration scale. Dysphagia. 2017;32(5):601–16. https://doi.org/10.1007/s00455-017-9809-z.
Patel JA, Ray BJ, Fernandez-Salvador C, Gouveia C, Zaghi S, Camacho M. Neuromuscular function of the soft palate and uvula in snoring and obstructive sleep apnea: a systematic review. Am J Otolaryngol. 2018;39(3):327–37. https://doi.org/10.1016/j.amjoto.2018.03.006.
Bhutada AM, Broughton WA, Garand KLF. Obstructive sleep apnea syndrome (OSAS) and swallowing function—a systematic review. Sleep and Breathing. 2020;24(3):791–9. https://doi.org/10.1007/s11325-020-02037-w.
Jardine M, Miles A, Allen J. Dysphagia onset in older adults during unrelated hospital admission: quantitative videofluoroscopic measures. Geriatrics (Basel). 2018;3(4):66. https://doi.org/10.3390/geriatrics3040066.
Jardine M, Miles A, Allen JE. Swallowing function in advanced age. Curr Opin Otolaryngol Head Neck Surg. 2018;26(6):367–74. https://doi.org/10.1097/MOO.0000000000000485.
Giraldo-Cadavid LF, Leal-Leaño LR, Leon-Basantes GA, Bastidas AR, Garcia R, Ovalle S, Abondano-Garavito JE. Accuracy of endoscopic and videofluoroscopic evaluations of swallowing for oropharyngeal dysphagia. Laryngoscope. 2017;127(9):2002–10. https://doi.org/10.1002/lary.26419.
Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and of pharyngeal dysphagia: changes over the years. Dysphagia. 2017;32(1):27–38. https://doi.org/10.1007/s00455-016-9775-x.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Non-existent.
Ethical Approval
The study was approved by the research ethics committee of Hospital Universitário Clementino Fraga Filho (HUCFF): Number 1.890.776.
Informed Consent
Participation in the study was voluntary, and all participants signed the informed consent form (ICF).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ferreira, F.R., Borges, T.G.V., Muniz, C.R. et al. Fiberoptic Endoscopic Evaluation of Swallowing in Resistant Hypertensive Patients With and Without Sleep Obstructive Apnea. Dysphagia 37, 1247–1257 (2022). https://doi.org/10.1007/s00455-021-10380-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10380-7