Abstract
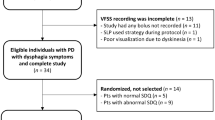
Agreement between self-reported dysphagic symptoms and actual swallowing physiology can vary widely across individuals. The Eating Assessment Tool-10 (EAT-10) is a self-report questionnaire commonly used to identify individuals with oropharyngeal dysphagia, but its interpretation for highly prevalent populations is poorly defined. Our primary objective was to determine if correlation strength between EAT-10 and Penetration–Aspiration Scale (PAS) scores differed by dysphagia etiology. Our secondary objective was to identify clinical factors that were associated with a mismatch between EAT-10 scores and videofluoroscopic findings. Outpatients with Parkinson disease (PD), stroke, and/or head and neck cancer (HNC) who completed EAT-10 and underwent videofluoroscopy were included (n = 203). EAT-10/PAS correlations were calculated by dysphagia etiology. We found that across the sample, higher EAT-10 scores were significantly correlated to higher PAS scores (rs = 0.31, p < 0.001). EAT-10 and PAS were moderately correlated in the HNC group (rs = 0.41, p < 0.001, n = 87), but correlations were modest in the PD (rs = 0.18, n = 41) and stroke groups (rs = 0.12, n = 59). Clinical characteristics of individuals with a “matched” profile (normal EAT-10 score and normal swallow physiology) and a “mismatched” profile (normal EAT-10 score and abnormal swallow physiology) were also compared. Individuals with a “mismatched” EAT-10/PAS profile appeared to be significantly older and had a worse Charlson Comorbidity Index than individuals with a “matched” profile. Within the HNC subgroup, EAT-10/PAS correlations for specific tumor sites, treatment types, and time since treatment are reported. Clinicians may consider these aspiration risk profiles when making recommendations for instrumented swallowing assessment.

Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Francis DO, Weymuller EA, Parvathaneni U, Merati AL, Yueh B. Dysphagia, stricture, and pneumonia in head and neck cancer patients: does treatment modality matter? Ann Otol Rhinol Laryngol. 2010; 119: 391–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20583737
Wermuth L, Stenager EN, Stenager E, Boldsen J. Mortality in patients with Parkinson’s disease. Acta Neurol Scand. 1995;92(1):55–8.
Miller N, Allcock L, Hildreth AJ, Jones D, Noble E, Burn DJ. Swallowing problems in Parkinson disease: frequency and clinical correlates. J Neurol Neurosurg Psychiatry. 2009;80:1047–9.
Parker C, Power M, Hamdy S, Bowen A, Tyrrell P, Thompson DG. Awareness of Dysphagia by patients following stroke predicts swallowing performance. Dysphagia. 2004;19(1):28–35.
Rogus-Pulia NM, Pierce MC, Mittal BB, Zecker SG, Logemann JA. Changes in swallowing physiology and patient perception of swallowing function following chemoradiation for head and neck cancer. Dysphagia. 2014;29(2):223–33.
Giraldo-Cadavid LF, Gutierrez-Achury AM, Ruales-Suarez K, Rengifo-Varona ML, Barros C, Posada A, et al. Validation of the Spanish Version of the Eating Assessment Tool-10 (EAT-10spa) in Colombia. A blinded prospective cohort study. Dysphagia. 2016;31:398–406.
Demir N, Serel Arslan S, İnal Ö, Karaduman AA. Reliability and validity of the Turkish Eating Assessment Tool (T-EAT-10). Dysphagia. 2016;31(5):644–9.
Wilmskoetter J, Bonilha H, Hong I, Hazelwood RJ, Martin-Harris B, Velozo C. Construct validity of the Eating Assessment Tool (EAT-10). Disabil Rehabil. 2017. https://doi.org/10.1080/09638288.2017.1398787.
Izaola O, Gómez Hoyos E, López JJ, Ortola A, Torres B, Primo D, et al. The 10-item eating assessment tool is associated with nutritional status, mortality and hospital stay in elderly individuals requiring hospitalization with acute diseases. Nutr Hosp. 2018. https://doi.org/10.20960/nh.1698.
Popman A, Richter M, Allen J, Wham C. High nutrition risk is associated with higher risk of dysphagia in advanced age adults newly admitted to hospital. Nutr Diet. 2018. https://doi.org/10.1111/1747-0080.12385.
Wakabayashi H, Matsushima M. Dysphagia assessed by the 10-item eating assessment tool is associated with nutritional status and activities of daily living in elderly individuals requiring long-term care. J Nutr Heal Aging. 2016;20:22–7.
Matsuo H, Yoshimura Y, Ishizaki N, Ueno T. Dysphagia is associated with functional decline during acute-care hospitalization of older patients. Geriatr Gerontol Int. 2017;17(10):1610–6.
Arrese LC, Carrau R, Plowman EK. Relationship between the eating assessment tool-10 and objective clinical ratings of swallowing function in individuals with head and neck cancer. Dysphagia. 2017;32:83–9.
Printza A, Kyrgidis A, Pavlidou E, Triaridis S, Constantinidis J. Reliability and validity of the Eating Assessment Tool-10 (Greek adaptation) in neurogenic and head and neck cancer-related oropharyngeal dysphagia. Eur Arch Oto-Rhino-Laryngol. 2018;275(7):1861–8.
Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, et al. Reliability and validity of the italian eating assessment tool. Ann Otol Rhinol Laryngol. 2013;122:717–24.
Rodrigues B, Nóbrega AC, Sampaio M, Argolo N, Melo A. Silent saliva aspiration in Parkinson’s disease. Mov Disord. 2011;26:138–41.
Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia. 2005;20:218–25.
Kendall KA, Ellerston J, Heller A, Houtz DR, Zhang C, Presson AP. Objective measures of swallowing function applied to the dysphagia population: a one year experience. Dysphagia. 2016;31(4):538–46.
Cheney DM, Tausif Siddiqui M, Litts JK, Kuhn MA, Belafsky PC. The ability of the 10-item eating assessment tool (EAT-10) to predict aspiration risk in persons with dysphagia. Ann Otol Rhinol Laryngol. 2015;124:351–4.
Arslan SS, Demir N, Kilinç HE, Karaduman AA. The ability of the eating assessment Tool-10 to detect aspiration in patients with neurological disorders. J Neurogastroenterol Motil. 2017;23(4):550–4.
Zuniga SA, Ebersole B, Jamal N. Utility of Eating Assessment Tool-10 in predicting aspiration in patients with unilateral vocal fold paralysis. Otolaryngol Head Neck Surg (United States). 2018;159(1):92–6.
Ding R, Logemann JA. Patient self-perceptions of swallowing difficulties as compared to expert ratings of videofluorographic studies. Folia Phoniatr Logop. 2008;59:39–52.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med Care. 2005;43:1130–9.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24.
Speyer R, Kertscher B, Cordier R. Functional health status in oropharyngeal dysphagia. J Gastroenterol Hepatol Res. 2014;3:1043–8.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Cramer D. Fundamental Statistics for Social Research. Fundam Stat Soc Res 2003.
Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. 1965;52:591–611.
Ware JE, Kosinski M, Keller SD. How to score the SF-12 physical and mental health summary scales. Second. Lincoln, RI Qual Metric. Boston: The Health Institute, New England Medical Center; 1998.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60.
Risk factors for oral cavity and oropharyngeal cancers [Internet]. Centers Dis. Control Prev. 2018. Available from: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/risk-factors.html
Mirghani H, Amen F, Moreau F, Lacau St Guily J. Do high-risk human papillomaviruses cause oral cavity squamous cell carcinoma? Oral Oncol. 2015;51(3):229–36.
Namasivayam-MacDonald AM, Steele CM, Keller HH. Perception versus performance of swallow function in residents of long-term care. Am J Speech-Language Pathol. 2019;28(3):1198–205.
Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20:600–7.
Acknowledgements
The authors sincerely thank Elisa R. Derickson, BA, for her assistance with the outcomes database.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was completed at Northern Arizona University and University of Wisconsin-Madison.
Rights and permissions
About this article
Cite this article
Bartlett, R.S., Kenz, M.K., Wayment, H.A. et al. Correlation Between EAT-10 and Aspiration Risk Differs by Dysphagia Etiology. Dysphagia 37, 11–20 (2022). https://doi.org/10.1007/s00455-021-10244-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10244-0