Abstract
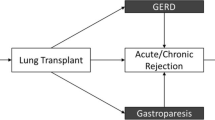
Gastroesophageal reflux disease and esophageal dysmotility are common in patients with advanced lung disease (ALD) and are associated with worse outcomes. Assessing esophageal function in these patients is relevant for determining pulmonary transplant eligibility and prognosticating post-transplant outcomes. Barium Swallow (BaS) is a non-invasive testing modality often performed as a complement to formal esophageal function tests (EFTs), but its role and clinical utility in this context is unknown. Therefore, we aimed to determine the relationship between BaS and EFTs with high-resolution manometry (HRM) and 24-h ambulatory pH-metry in patients with ALD. We performed a retrospective study of 226 consecutive patients undergoing evaluation for lung transplantation at a single center. All patients underwent EFTs and BaS independent of clinical history or symptoms per institutional protocol. Appropriate statistical tests were performed to evaluate the relationship between EFTs and BaS. Mucosal, reflux and motility findings were categorized. Abnormal motility was reported in 133 (59%) patients by BaS and 99 (44%) by HRM, with a significant difference in the proportions of patients with abnormal studies (p < 0.01). There were 7 (26%) patients with abnormal barium tablet passage who had normal HRM. The sensitivity (35%) and specificity (77%) for detecting pathologic reflux with BaS was poor. Inducibility of reflux and barium column height were not associated with pH-metry results. No clinically significant luminal irregularities were identified. In conclusion, while BaS can non-invasively assess esophageal mucosa, its findings are not associated with EFTs in patients with ALD.

Similar content being viewed by others
Change history
09 May 2020
The original version of this article unfortunately contained a mistake. The shared first authorship information was missing in the published article. It has been given below. The first authorship is shared between Dr. Shai Posner and Kurren Mehta
References
Johannson KA, Strambu I, Ravaglia C, Grutters JC, Valenzuela C, Mogulkoc N, Luppi F, Richeldi L, Wells AU, Vancheri C, Kreuter M. Antacid therapy in idiopathic pulmonary fibrosis: more questions than answers? Lancet Resp Med. 2017;5:591–8.
D'Ovidio F, Mura M, Tsang M, Waddell TK, Hutcheon MA, Singer LG, Hadjiliadis D, Chaparro C, Gutierrez C, Pierre A, Darling G, Liu M, Keshavjee S. Bile acid aspiration and the development of bronchiolitis obliterans after lung transplantation. J Thoracic Cardiovas Surgery. 2005;129:1144–52.
D'Ovidio F, Mura M, Ridsdale R, Takahashi H, Waddell TK, Hutcheon M, Hadjiliadis D, Singer LG, Pierre A, Chaparro C, Gutierrez C, Miller L, Darling G, Liu M, Post M, Keshavjee S. The effect of reflux and bile acid aspiration on the lung allograft and its surfactant and innate immunity molecules SP-A and SP-D. Am J Transplantation : Official J Am Soci Transplant Am Soci Transplant Surgeons. 2006;6:1930–8.
Fisichella PM, Davis CS, Lowery E, Ramirez L, Gamelli RL, Kovacs EJ. Aspiration, localized pulmonary inflammation, and predictors of early-onset bronchiolitis obliterans syndrome after lung transplantation. J Am College Surgeons. 2013;217:90–100.
Tobin RW, Pope CE, Pellegrini CA, Emond MJ, Sillery J, Raghu G. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;158:1804–8.
Elserag HB, Sonnenberg A. Comorbid occurrence of laryngeal or pulmonary disease with esophagitis in United States military veterans. Gastroenterology. 1997;113:755–60.
Raghu G, Freudenberger TD, Yang S, Curtis JR, Spada C, Hayes J, Sillery JK, Pope CE 2nd, Pellegrini CA. High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. European Respiratory J. 2006;27:136–42.
Seccombe J, Mirza F, Hachem R, Gyawali CP. Esophageal motor disease and reflux patterns in patients with advanced pulmonary disease undergoing lung transplant evaluation. Neurogastroenterology Motility. 2013;25:657–63.
Basseri B, Conklin JL, Pimentel M, Tabrizi R, Phillips EH, Simsir SA, Chaux GE, Falk JA, Ghandehari S, Soukiasian HJ. Esophageal motor dysfunction and gastroesophageal reflux are prevalent in lung transplant candidates. Annals Thoracic Surgery. 2010;90:1630–6.
D'Ovidio F, Singer LG, Hadjiliadis D, Pierre A, Waddell TK, de Perrot M, Hutcheon M, Miller L, Darling G, Keshavjee S. Prevalence of gastroesophageal reflux in end-stage lung disease candidates for lung transplant. Annals Thoracic Surgery. 2005;80:1254–60.
Posner S, Zheng J, Wood RK, Shimpi RA, Hartwig MG, Chow SC, Leiman DA. Gastroesophageal reflux symptoms are not sufficient to guide esophageal function testing in lung transplant candidates. Diseases of the esophagus Official J Int Soc Diseases Esophagus. 2018. https://doi.org/10.1093/dote/dox157.
Sweet MP, Herbella FA, Leard L, Hoopes C, Golden J, Hays S, Patti MG. The prevalence of distal and proximal gastroesophageal reflux in patients awaiting lung transplantation. Ann Surg. 2006;244:491–7.
Tangaroonsanti A, Vela MF, Crowell MD, DeVault KR. Houghton LA Esophageal dysmotility according to Chicago classification v.30 vs v.20: Implications for association with reflux, bolus clearance, and allograft failure post-lung transplantation. Neurogastroenterol Motility Official J Eu Gastrointestinal Motility Society. 2018;30:13296.
Katzka DA. A gastroenterologist's perspective on the role of barium esophagography in gastroesophageal reflux disease. Abdominal radiology (New York). 2018;43:1319–22.
Schima W, Eisenhuber E, Kulinna-Cosentini C (2011) Radiologic evaluation of esophageal function. Dysphagia: Springer, pp 339–357.
Levine MS, Rubesin SE, Laufer IJR. Barium studies in modern radiology: do they have a role? Radiology. 2009;250:18–22.
Mendez BM, Davis CS, Weber C, Joehl RJ, Fisichella PM. Gastroesophageal reflux disease in lung transplant patients with cystic fibrosis. Am J Surg. 2012;204:e21–26.
Seccombe J, Mirza F, Hachem R, Gyawali CJN, Esophageal motor disease and reflux patterns in patients with advanced pulmonary disease undergoing lung transplant evaluation. Neurogastroenterol Motil. 2013;25:657–e508.
Bello B, Zoccali M, Gullo R, Allaix ME, Herbella FA, Gasparaitis A, Patti MG. Gastroesophageal reflux disease and antireflux surgery-what is the proper preoperative work-up? J Gastrointestinal Surg: Official J Soc Surgery Alimentary Tract. 2013;17:14–20.
Serna-Gallegos D, Basseri B, Bairamian V, Pimentel M, Soukiasian HJ. Gastroesophageal reflux reported on esophagram does not correlate with pH monitoring and high-resolution esophageal manometry. The American surgeon. 2014;80:1026–9.
Halland M, Ravi K, Barlow J, Arora A. Correlation between the radiological observation of isolated tertiary waves on an esophagram and findings on high-resolution esophageal manometry. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2016;29:22–6.
O'Rourke AK, Lazar A, Murphy B, Castell DO, Martin-Harris B. Utility of Esophagram versus High-Resolution Manometry in the Detection of Esophageal Dysmotility. Otolaryngology-head Neck Surgery official J Am Academy Otolaryngology-Head and Neck Surgery. 2016;154:888–91.
Posner S, Finn RT, Shimpi RA, Wood RK, Fisher D, Hartwig MG, Klapper J, Reynolds J, Niedzwiecki D, Parish A, Leiman DA. Esophageal contractility increases and gastroesophageal reflux does not worsen after lung transplantation. Dis Esophagus : official journal of the International Society for Diseases of the Esophagus. 2019;32(10):1–8.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterology Motility. 2015;27:160–74.
Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:527–33.
Blonski W, Kumar A, Feldman J, Richter JE. Timed Barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018;113:196–203.
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJ. Relationship between esophageal contraction patterns and clearance of swallowed liquid and solid boluses in healthy controls and patients with dysphagia. Neurogastroenterol Motility. 2012;24:e364–372.
Ott DJ, Richter JE, Chen YM, Wu WC, Gelfand DW, Castell DO. Esophageal radiography and manometry: correlation in 172 patients with dysphagia. AJR Am J Roentgenol. 1987;149:307–11.
El-Takli I, O'Brien P, Paterson WG. Clinical diagnosis of achalasia: how reliable is the barium x-ray? Can J Gastroenterol. 2006;20:335–7.
Lacy BE, Weiser K, Chertoff J, Fass R, Pandolfino JE, Richter JE, Rothstein RI, Spangler C, Vaezi MF. The diagnosis of gastroesophageal reflux disease. Am J Medicine. 2010;123:583–92.
Pan JJ, Levine MS, Redfern RO, Rubesin SE, Laufer I, Katzka DA. Gastroesophageal reflux: comparison of barium studies with 24-h pH monitoring. Eur J Radiol. 2003;47:149–53.
Hartwig MG, Anderson DJ, Onaitis MW, Reddy S, Snyder LD, Lin SS, Davis RD. Fundoplication after lung transplantation prevents the allograft dysfunction associated with reflux. Annals Thoracic Surgery. 2011;92:462–8.
Sweet MP, Patti MG, Hoopes C, Hays SR, Golden JA. Gastro-oesophageal reflux and aspiration in patients with advanced lung disease. Thorax. 2009;64:167–73.
Raghu G, Pellegrini CA, Yow E, Flaherty KR, Meyer K, Noth I, Scholand MB, Cello J, Ho LA, Pipavath S, Lee JS, Lin J, Maloney J, Martinez FJ, Morrow E, Patti MG, Rogers S, Wolters PJ, Yates R, Anstrom KJ, Collard HR. Laparoscopic anti-reflux surgery for the treatment of idiopathic pulmonary fibrosis (WRAP-IPF): a multicentre, randomised, controlled phase 2 trial. Lancet Respiratory Medicine. 2018;6:707–14.
Weitzendorfer M, Kohler G, Antoniou SA, Pallwein-Prettner L, Manzenreiter L, Schredl P, Emmanuel K, Koch OO. Preoperative diagnosis of hiatal hernia: barium swallow X-ray, high-resolution manometry, or endoscopy? European Surgery. 2017;49:210–7.
Acknowledgements
The authors thank Richard K. Wood (RKW) and Rahul A. Shimpi (RAS) for their esophageal function test interpretations.
Funding
No grant support was used to fund this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Posner, S., Mehta, K., Parish, A. et al. Esophageal Function Tests are Not Associated with Barium Swallow Findings in Advanced Lung Disease. Dysphagia 35, 864–870 (2020). https://doi.org/10.1007/s00455-020-10113-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10113-2