Abstract
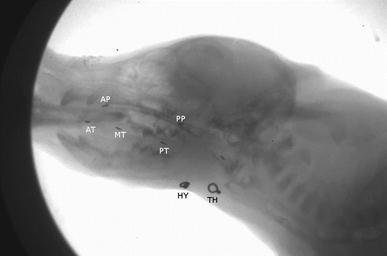
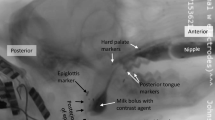
Muscle injury is a frequent side effect of radiation treatment for head and neck cancer. To understand the pathophysiology of injury-related dysfunction, we investigated the effects of a single muscle injury to the mylohyoid on oropharyngeal swallowing function in the rat. The mylohyoid protects the airway from food/liquid via hyolaryngeal elevation and plays an active role during both oral and pharyngeal swallowing. We hypothesized (1) that fibrosis to the mylohyoid alters swallowing bolus flow and licking patterns and (2) that injury to the mylohyoid changes normal activity of submental, laryngeal, and pharyngeal muscles during swallowing. A chilled cryoprobe was applied to the rat mylohyoid muscle to create a localized injury. One and two weeks after injury, swallowing bolus transit was assessed via videofluoroscopy and licking behavior via an electrical lick sensor. The motor activity of five swallow-related muscles was analyzed immediately after injury using electromyography (EMG). Comparisons were made pre- and post-injury. Fibrosis was confirmed in the mylohyoid at 2 weeks after injury by measuring collagen content. One week after injury, bolus size decreased, swallowing rate reduced, and licking patterns were altered. Immediately post-injury, there was a significant depression in mylohyoid and thyropharyngeus EMG amplitudes during swallowing. Our results demonstrated that injury to the mylohyoid is sufficient to cause changes in deglutition. These disruptions in oral and pharyngeal swallowing were detected prior to long-term fibrotic changes, including delays in tongue movement, alterations in bolus flow, and changes in sensorimotor function. Therefore, injuring a single important swallowing muscle can have dramatic clinical effects.





Similar content being viewed by others
References
Kotz T, Costello R, Li Y, Posner MR. Swallowing dysfunction after chemoradiation for advanced squamous cell carcinoma of the head and neck. Head Neck. 2004;26(4):365–72. https://doi.org/10.1002/hed.10385.
Van den Steen L, Van Gestel D, Vanderveken O, Vanderwegen J, Lazarus C, Daisne JF, Van Laer C, Specenier P, Van Rompaey D, Marien S, Lawson G, Chantrain G, Gauthier D, Van den Weyngaert D, Cvilic S, Beauvois S, Allouche J, Delacroix L, Vermorken JB, Peeters M, Dragan T, Van de Heyning P, De Bodt M, Van Nuffelen G. Evolution of self-perceived swallowing function, tongue strength and swallow-related quality of life during radiotherapy in head and neck cancer patients. Head Neck. 2019;26(4):365–72. https://doi.org/10.1002/hed.25684.
Kendall KA, McKenzie SW, Leonard RJ, Jones CU. Timing of swallowing events after single-modality treatment of head and neck carcinomas with radiotherapy. Ann Otol Rhinol Laryngol. 2000;109(8):767–75. https://doi.org/10.1177/000348940010900812.
Kendall KA, Tanner K, Kosek SR. Timing of events during deglutition after chemoradiation therapy for oropharyngeal carcinoma. Head Neck. 2014;37(8):1193–9. https://doi.org/10.1002/hed.23735.
Lazarus C, Logemann JA, Gibbons P. Effects of maneuvers on swallowing function in a dysphagic oral cancer patient. Head Neck. 1993;15(5):419–24.
McClelland S 3rd, Andrews JZ, Chaudhry H, Teckie S, Goenka A. Prophylactic versus reactive gastrostomy tube placement in advanced head and neck cancer treated with definitive chemoradiotherapy: a systematic review. Oral Oncol. 2018;87:77–81. https://doi.org/10.1016/j.oraloncology.2018.10.028.
Popovtzer A, Cao Y, Feng FY, Eisbruch A. Anatomical changes in the pharyngeal constrictors after chemo-irradiation of head and neck cancer and their dose-effect relationships: MRI-based study. Radiother Oncol. 2009;93(3):510–5. https://doi.org/10.1016/j.radonc.2009.05.013.
Eisele DW, Koch DG, Tarazi AE, Jones B. Case report: aspiration from delayed radiation fibrosis of the neck. Dysphagia. 1991;6(2):120–2.
Hutcheson KA, Lewin JS, Barringer DA, Lisec A, Gunn GB, Moore MW, Holsinger FC. Late dysphagia after radiotherapy-based treatment of head and neck cancer. Cancer. 2012;118(23):5793–9. https://doi.org/10.1002/cncr.27631.
Ekberg O, Nylander G. Pharyngeal dysfunction after treatment for pharyngeal cancer with surgery and radiotherapy. Gastrointest Radiol. 1983;8(2):97–104.
Starmer HM. Dysphagia in head and neck cancer: prevention and treatment. Curr Opin Otolaryngol Head Neck Surg. 2014;22(3):195–200. https://doi.org/10.1097/MOO.0000000000000044.
Ozkaya Akagunduz O, Eyigor S, Kirakli E, Tavlayan E, Erdogan Cetin Z, Kara G, Esassolak M. Radiation-associated chronic dysphagia assessment by flexible endoscopic evaluation of swallowing (FEES) in head and neck cancer patients: swallowing-related structures and radiation dose-volume effect. Ann Otol Rhinol Laryngol. 2019;128(2):73–84. https://doi.org/10.1177/0003489418804260.
Kumar R, Madanikia S, Starmer H, Yang W, Murano E, Alcorn S, McNutt T, Le Y, Quon H. Radiation dose to the floor of mouth muscles predicts swallowing complications following chemoradiation in oropharyngeal squamous cell carcinoma. Oral Oncol. 2014;50(1):65–70. https://doi.org/10.1016/j.oraloncology.2013.10.002.
Russell JA, Connor NP. Effects of age and radiation treatment on function of extrinsic tongue muscles. Radiat Oncol. 2014;9:254. https://doi.org/10.1186/s13014-014-0254-y.
Benedict PA, Ruiz R, Verma A, Dion GR, Oh P, Wang B, Ahmed OH, Hiwatashi N, Bing R, Victor K, Hu KS, Johnson A, Branski RC, Amin MR. The effects of concurrent chemoradiation therapy to the base of tongue in a preclinical model. Laryngoscope. 2018;128(8):1783–90. https://doi.org/10.1002/lary.27033.
Starmer HM, Quon H, Kumar R, Alcorn S, Murano E, Jones B, Humbert I. The effect of radiation dose on swallowing: evaluation of aspiration and kinematics. Dysphagia. 2015;30(4):430–7. https://doi.org/10.1007/s00455-015-9618-1.
Lehr RP, Blanton PL, Biggs NL. An electromyographic study of the mylohyoid muscle. Anat Rec. 1971;169(4):651–60. https://doi.org/10.1002/ar.1091690405.
Thexton AJ, Crompton AW, German RZ. Electromyographic activity during the reflex pharyngeal swallow in the pig: Doty and Bosma 1956 revisited. J Appl Physiol. 2007;102(2):587–600. https://doi.org/10.1152/japplphysiol.00456.2006.
Thexton AJ, Crompton AW. German RZ. EMG activity in hyoid muscles during pig suckling. J Appl Physiol. 2012;112(9):1512–9. https://doi.org/10.1152/japplphysiol.00450.2011.
van Eijden TM, Koolstra JH. A model for mylohyoid muscle mechanics. J Biomech. 1998;31(11):1017–24.
Pearson WG Jr, Langmore SE, Zumwalt AC. Evaluating the structural properties of suprahyoid muscles and their potential for moving the hyoid. Dysphagia. 2011;26(4):345–51. https://doi.org/10.1007/s00455-010-9315-z.
Jafari S, Prince RA, Kim DY, Paydarfar D. Sensory regulation of swallowing and airway protection: a role for the internal superior laryngeal nerve in humans. J Physiol. 2003;550(Pt 1):287–304. https://doi.org/10.1113/jphysiol.2003.039966.
Holman SD, Waranch DR, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Lukasik SL, German RZ. Sucking and swallowing rates after palatal anesthesia: an electromyographic study in infant pigs. J Neurophysiol. 2013;110(2):387–96. https://doi.org/10.1152/jn.00064.2013.
Hu JW. Response properties of nociceptive and non-nociceptive neurons in the rat's trigeminal subnucleus caudalis (medullary dorsal horn) related to cutaneous and deep craniofacial afferent stimulation and modulation by diffuse noxious inhibitory controls. Pain. 1990;41(3):331–45.
Sessle BJ, Hu JW, Amano N, Zhong G. Convergence of cutaneous, tooth pulp, visceral, neck and muscle afferents onto nociceptive and non-nociceptive neurones in trigeminal subnucleus caudalis (medullary dorsal horn) and its implications for referred pain. Pain. 1986;27(2):219–35.
Tsujimura T, Kitagawa J, Ueda K, Iwata K. Inhibition of swallowing reflex following phosphorylation of extracellular signal-regulated kinase in nucleus tractus solitarii neurons in rats with masseter muscle nociception. Neurosci Lett. 2009;450(3):361–4. https://doi.org/10.1016/j.neulet.2008.12.008.
Tsujimura T, Kondo M, Kitagawa J, Tsuboi Y, Saito K, Tohara H, Ueda K, Sessle BJ, Iwata K. Involvement of ERK phosphorylation in brainstem neurons in modulation of swallowing reflex in rats. J Physiol. 2009;587(Pt 4):805–17. https://doi.org/10.1113/jphysiol.2008.165324.
van Amerongen MJ, Harmsen MC, Petersen AH, Popa ER, van Luyn MJ. Cryoinjury: a model of myocardial regeneration. Cardiovasc Pathol. 2008;17(1):23–31. https://doi.org/10.1016/j.carpath.2007.03.002.
van Amerongen MJ, Harmsen MC, van Rooijen N, Petersen AH, van Luyn MJ. Macrophage depletion impairs wound healing and increases left ventricular remodeling after myocardial injury in mice. Am J Pathol. 2007;170(3):818–29. https://doi.org/10.2353/ajpath.2007.060547.
Somogyi GT, Yokoyama T, Szell EA, Smith CP, de Groat WC, Huard J, Chancellor MB. Effect of cryoinjury on the contractile parameters of bladder strips: a model of impaired detrusor contractility. Brain Res Bull. 2002;59(1):23–8.
Alves AN, Fernandes KP, Melo CA, Yamaguchi RY, Franca CM, Teixeira DF, Bussadori SK, Nunes FD, Mesquita-Ferrari RA. Modulating effect of low level-laser therapy on fibrosis in the repair process of the tibialis anterior muscle in rats. Lasers Med Sci. 2014;29(2):813–21. https://doi.org/10.1007/s10103-013-1428-9.
Neel HB, Farrell KH, DeSanto LW, Payne WS, Sanderson DR. Cryosurgery of respiratory structures. I. Cryonecrosis of trachea and bronchus. Laryngoscope 1973;83(7):1062–1071. https://doi.org/10.1288/00005537-197307000-00007.
Hsu HY, Chai CY, Lee MS. Radiation-induced muscle damage in rats after fractionated high-dose irradiation. Radiat Res. 1998;149(5):482–6.
Strungs EG, Ongstad EL, O'Quinn MP, Palatinus JA, Jourdan LJ, Gourdie RG. Cryoinjury models of the adult and neonatal mouse heart for studies of scarring and regeneration. Methods Mol Biol. 2013;1037:343–53. https://doi.org/10.1007/978-1-62703-505-7_20.
Rasband WS. ImageJ. https://imagej.nih.gov/ij/.
Lever TE, Braun SM, Brooks RT, Harris RA, Littrell LL, Neff RM, Hinkel CJ, Allen MJ, Ulsas MA. Adapting human videofluoroscopic swallow study methods to detect and characterize dysphagia in murine disease models. JoVE. 2015;97:e52319. https://doi.org/10.3791/52319.
Russell JA, Ciucci MR, Hammer MJ, Connor NP. Videofluorographic assessment of deglutitive behaviors in a rat model of aging and Parkinson disease. Dysphagia. 2013;28(1):95–104. https://doi.org/10.1007/s00455-012-9417-x.
Weijnen JA. Licking behavior in the rat: measurement and situational control of licking frequency. Neurosci Biobehav Rev. 1998;22(6):751–60.
Lin XB, Pierce DR, Light KE, Hayar A. The fine temporal structure of the rat licking pattern: what causes the variabiliy in the interlick intervals and how is it affected by the drinking solution? Chem Senses. 2013;38(8):685–704. https://doi.org/10.1093/chemse/bjt038.
Davis JD, Smith GP. Analysis of the microstructure of the rhythmic tongue movements of rats ingesting maltose and sucrose solutions. Behav Neurosci. 1992;106(1):217–28.
Davis JD, Smith GP, Kung TM. Abdominal vagotomy alters the structure of the ingestive behavior of rats ingesting liquid diets. Behav Neurosci. 1994;108(4):767–79.
Spector AC, Klumpp PA, Kaplan JM. Analytical issues in the evaluation of food deprivation and sucrose concentration effects on the microstructure of licking behavior in the rat. Behav Neurosci. 1998;112(3):678–94.
Spearman DG, Poliacek I, Rose MJ, Bolser DC, Pitts T. Variability of the pharyngeal phase of swallow in the cat. PLoS ONE. 2014;9(8):e106121–e106121106121. https://doi.org/10.1371/journal.pone.0106121.
Miyabara EH, Martin JL, Griffin TM, Moriscot AS, Mestril R. Overexpression of inducible 70-kDa heat shock protein in mouse attenuates skeletal muscle damage induced by cryolesioning. Am J Physiol Cell Physiol. 2006;290(4):C1128–1138. https://doi.org/10.1152/ajpcell.00399.2005.
Nakamura J-i, Miyaoka Y, Takagi M. Influences of tongue protrusion on rhythmical jaw movement in rats. J Oral Biosci. 2007;49(4):269–77. https://doi.org/10.1016/S1349-0079(07)80022-3.
Ding P, Fung GS, Lin M, Holman SD, German RZ. The effect of bilateral superior laryngeal nerve lesion on swallowing: a novel method to quantitate aspirated volume and pharyngeal threshold in videofluoroscopy. Dysphagia. 2015;30(1):47–56. https://doi.org/10.1007/s00455-014-9572-3.
Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258(5 Pt 1):G675–681. https://doi.org/10.1152/ajpgi.1990.258.5.G675.
Butler SG, Stuart A, Castell D, Russell GB, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume on pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52(1):240–53. https://doi.org/10.1044/1092-4388(2008/07-0092).
Hoffman MR, Ciucci MR, Mielens JD, Jiang JJ, McCulloch TM. Pharyngeal swallow adaptations to bolus volume measured with high-resolution manometry. Laryngoscope. 2010;120(12):2367–73. https://doi.org/10.1002/lary.21150.
Gould FDH, Yglesias B, Ohlemacher J, German RZ. Pre-pharyngeal swallow effects of recurrent laryngeal nerve lesion on bolus shape and airway protection in an infant pig model. Dysphagia. 2017;32(3):362–73. https://doi.org/10.1007/s00455-016-9762-2.
Humbert IA, Lokhande A, Christopherson H, German R, Stone A. Adaptation of swallowing hyo-laryngeal kinematics is distinct in oral vs. pharyngeal sensory processing. J Appl Physiol 2012;112(10):1698–1705. https://doi.org/10.1152/japplphysiol.01534.2011.
Hughes TA, Wiles CM. Clinical measurement of swallowing in health and in neurogenic dysphagia. QJM. 1996;89(2):109–16.
Eisbruch A, Lyden T, Bradford CR, Dawson LA, Haxer MJ, Miller AE, Teknos TN, Chepeha DB, Hogikyan ND, Terrell JE, Wolf GT. Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2002;53(1):23–8.
Pauloski BR, Logemann JA. Impact of tongue base and posterior pharyngeal wall biomechanics on pharyngeal clearance in irradiated postsurgical oral and oropharyngeal cancer patients. Head Neck. 2000;22(2):120–31.
Logemann JA, Rademaker AW, Pauloski BR, Lazarus CL, Mittal BB, Brockstein B, MacCracken E, Haraf DJ, Vokes EE, Newman LA, Liu D. Site of disease and treatment protocol as correlates of swallowing function in patients with head and neck cancer treated with chemoradiation. Head Neck. 2006;28(1):64–73. https://doi.org/10.1002/hed.20299.
Westergren A, Unosson M, Ohlsson O, Lorefalt B, Hallberg IR. Eating difficulties, assisted eating and nutritional status in elderly (%3e or = 65 years) patients in hospital rehabilitation. Int J Nurs Stud. 2002;39(3):341–51.
Austen JM, Strickland JA, Sanderson DJ. Memory-dependent effects on palatability in mice. Physiol Behav. 2016;167:92–9. https://doi.org/10.1016/j.physbeh.2016.09.001.
Ciubotariu A, Arendt-Nielsen L, Graven-Nielsen T. The influence of muscle pain and fatigue on the activity of synergistic muscles of the leg. Eur J Appl Physiol. 2004;91(5–6):604–14. https://doi.org/10.1007/s00421-003-1026-9.
Hodges PW, Ervilha UF, Graven-Nielsen T. Changes in motor unit firing rate in synergist muscles cannot explain the maintenance of force during constant force painful contractions. J Pain. 2008;9(12):1169–74. https://doi.org/10.1016/j.jpain.2008.06.012.
Contreras RJ, Beckstead RM, Norgren R. The central projections of the trigeminal, facial, glossopharyngeal and vagus nerves: an autoradiographic study in the rat. J Auton Nerv Syst. 1982;6(3):303–22.
Arendt-Nielsen L, Graven-Nielsen T. Muscle pain: sensory implications and interaction with motor control. Clin J Pain. 2008;24(4):291–8. https://doi.org/10.1097/AJP.0b013e31815b608f.
German RZ, Crompton AW, Thexton AJ. Variation in EMG activity: a hierarchical approach. Integr Comp Biol. 2008;48(2):283–93. https://doi.org/10.1093/icb/icn022.
Funding
NIH T35 DK072923 (Bonomo).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
King, S.N., Fletcher, B., Kimbel, B. et al. Adaptations to Oral and Pharyngeal Swallowing Function Induced by Injury to the Mylohyoid Muscle. Dysphagia 35, 814–824 (2020). https://doi.org/10.1007/s00455-019-10087-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10087-w