Abstract
Age-related physiological changes of the swallowing act impair particularly the oral phase and the tongue function, which is very important for bolus preparation and transfer. At present, there are no easily applicable methods for measurement of this phase of swallowing. This study was designed to investigate the deglutitive tongue movement by M-mode ultrasound and to compare the collected parameters of different age groups. In this exploratory prospective study, the tongue and its movements of 20 younger and 30 older women were examined during swallowing by B-mode and M-mode ultrasound. Preexisting dysphagia or malnutrition as well as psychic or neurological deficits were excluded by clinical examination and screening with the Mini Nutritional Assessment-Short Form (MNA-SF), the Gugging Swallowing Screen (GUSS), the Mini-Mental State Examination (MMSE) and the Barthel Index. The data were compared with each other and statistically analyzed. With increasing age, a change in the tongue movement pattern becomes apparent. In the group of older women, the vertical lingual movement had a smaller amplitude (p < 0.001) and a shorter time to the maximum amplitude (p < 0.03) than in the group of younger women. However, there were no differences in the tongue diameter (p > 0.4). The tongue movement pattern appears to be subject to age-specific changes, in contrast to anatomy. The use of M-mode ultrasonography is an easy, radiation-free and cost-effective method for the assessment of the oral phase of swallowing. Limitations are the widely scattered values of the ultrasound findings. Further studies are needed for validation and definition of standard values for this promising method.


Similar content being viewed by others
References
Nienstedt JC, Pflug C. Schluckstörungen—Altersbedingte Dysphagie frühzeitig erkennen. HNO Nachrichten. 2017;6(6):19–24. https://doi.org/10.1007/s00060-017-5556-x.
Shaker R, Lang IM. Effect of aging on the deglutitive oral, pharyngeal, and esophageal motor function. Dysphagia. 1994;9(4):221–8. https://doi.org/10.1007/bf00301914.
Jungheim M, Schwemmle C, Miller S, Kuhn D, Ptok M. Swallowing and dysphagia in the elderly. HNO. 2014;62(9):644–51. https://doi.org/10.1007/s00106-014-2864-y.
Muhle P, Wirth R, Glahn J, Dziewas R. Age-related changes in swallowing. Physiology and pathophysiology. Nervenarzt. 2015;86(4):440–51.
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc. 2013;61(3):418–22. https://doi.org/10.1111/jgs.12124.
Yoshikawa M, Yoshida M, Nagasaki T, Tanimoto K, Tsuga K, Akagawa Y, Komatsu T. Aspects of swallowing in healthy dentate elderly persons older than 80 years. J Gerontol A Biol Sci Med Sci. 2005;60(4):506–9.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30(1):80–7. https://doi.org/10.1007/s00455-014-9577-y.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50(5):M257–262.
Sheth N, Diner WC. Swallowing problems in the elderly. Dysphagia. 1988;2(4):209–15.
Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2(4):216–9.
Langmore SE. Evaluation of oropharyngeal dysphagia: which diagnostic tool is superior? Curr Opin Otolaryngol Head Neck Surg. 2003;11(6):485–9.
Logemann JA, Rademaker AW, Pauloski BR, Ohmae Y, Kahrilas PJ. Normal swallowing physiology as viewed by videofluoroscopy and videoendoscopy. Folia Phoniatr Logop. 1998;50(6):311–9. https://doi.org/10.1159/000021473.
Kidder TM, Langmore SE, Martin BJ. Indications and techniques of endoscopy in evaluation of cervical dysphagia: comparison with radiographic techniques. Dysphagia. 1994;9(4):256–61.
Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110(4):563–74. https://doi.org/10.1097/00005537-200004000-00008.
Shawker TH, Sonies B, Stone M, Baum BJ. Real-time ultrasound visualization of tongue movement during swallowing. J Clin Ultrasound. 1983;11(9):485–90.
Chi-Fishman G. Quantitative lingual, pharyngeal and laryngeal ultrasonography in swallowing research: a technical review. Clin Linguist Phon. 2005;19(6–7):589–604.
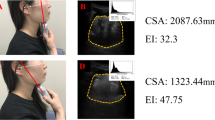
Li C, Li J, Zhang C, Cao X, Li N, Song D, Yu T. Application of B+M-mode ultrasonography in assessing deglutitive tongue movements in healthy adults. Med Sci Monit. 2015;21:1648–55. https://doi.org/10.12659/MSM.893591.
Peng CL, Miethke RR, Pong SJ, Lin CT. Investigation of tongue movements during swallowing with M-mode ultrasonography. J Orofac Orthop. 2007;68(1):17–25. https://doi.org/10.1007/s00056-007-0547-y.
Galen S, Jost-Brinkmann PG. B-mode and M-mode ultrasonography of tongue movements during swallowing. J Orofac Orthop. 2010;71(2):125–35. https://doi.org/10.1007/s00056-010-9928-8.
Crow HC, Ship JA. Tongue strength and endurance in different aged individuals. J Gerontol A 1996;51(5):M247–250.
Youmans SR, Youmans GL, Stierwalt JA. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24(1):57–655. https://doi.org/10.1007/s00455-008-9171-2.
Todd JT, Lintzenich CR, Butler SG. Isometric and swallowing tongue strength in healthy adults. Laryngoscope. 2013;123(10):2469–73. https://doi.org/10.1002/lary.23852.
Butler SG, Stuart A, Leng X, Wilhelm E, Rees C, Williamson J, Kritchevsky SB. The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol A 2011;66(4):452–8. https://doi.org/10.1093/gerona/glq234.
Trapl M, Enderle P, Nowotny M, Teuschl Y, Matz K, Dachenhausen A, Brainin M. Dysphagia bedside screening for acute-stroke patients: the gugging swallowing screen. Stroke. 2007;38(11):2948–52. https://doi.org/10.1161/STROKEAHA.107.483933.
Guigoz Y, Vellas BJ, Garry PJ. Mini Nutritional Assessment: a practical assessment tool for grading the nutritional state of elderly patients. Facts Res Gerontol. 1994;4(suppl 2):15–59.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC, Group MN-I. Validation of the mini nutritional assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–8.
Bauer JM, Kaiser MJ, Anthony P, Guigoz Y, Sieber CC. The Mini Nutritional assessment–its history, today's practice, and future perspectives. Nutr Clin Pract. 2008;23(4):388–96. https://doi.org/10.1177/0884533608321132.
Vellas B, Villars H, Abellan G, Soto ME, Rolland Y, Guigoz Y, Morley JE, Chumlea W, Salva A, Rubenstein LZ, Garry P. Overview of the MNA–its history and challenges. J Nutr Health Aging. 2006;10(6):456–63.
Creavin ST, Wisniewski S, Noel-Storr AH, Trevelyan CM, Hampton T, Rayment D, Thom VM, Nash KJ, Elhamoui H, Milligan R, Patel AS, Tsivos DV, Wing T, Phillips E, Kellman SM, Shackleton HL, Singleton GF, Neale BE, Watton ME, Cullum S (2016) Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev (1):CD011145.
Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3), 189–198.
Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965;14:61–5.
Hara K, Tohara H, Kobayashi K, Yamaguchi K, Yoshimi K, Nakane A, Minakuchi S. Age-related declines in the swallowing muscle strength of men and women aged 20–89 years: A cross-sectional study on tongue pressure and jaw-opening force in 980 subjects. Arch Gerontol Geriatr. 2018;78:64–70. https://doi.org/10.1016/j.archger.2018.05.015.
Hirai T, Tanaka O, Koshino H, Takasaki H, Hashikawa Y, Yajima T, Matai N (1989) Aging and tongue skill. Ultrasound (motion-mode) evaluation. Nihon Hotetsu Shika Gakkai Zasshi 33(2), 457–465.
Yabunaka K, Sanada H, Sanada S, Konishi H, Hashimoto T, Yatake H, Yamamoto K, Katsuda T, Ohue M. Sonographic assessment of hyoid bone movement during swallowing: a study of normal adults with advancing age. Radiol Phys Technol. 2011;4(1):73–7. https://doi.org/10.1007/s12194-010-0107-9.
Lang T, Cauley JA, Tylavsky F, Bauer D, Cummings S, Harris TB, Health ABCS. Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: the health, aging, and body composition study. J Bone Miner Res. 2010;25(3):513–9. https://doi.org/10.1359/jbmr.090807.
Andersen JL. Muscle fibre type adaptation in the elderly human muscle. Scand J Med Sci Sports. 2003;13(1):40–7.
Barber L, Scicchitano BM, Musaro A. Molecular and cellular mechanisms of muscle aging and sarcopenia and effects of electrical stimulation in seniors. Eur J Transl Myol. 2015;25(4):231–6. https://doi.org/10.4081/ejtm.2015.5227.
Machida N, Tohara H, Hara K, Kumakura A, Wakasugi Y, Nakane A, Minakuchi S. Effects of aging and sarcopenia on tongue pressure and jaw-opening force. Geriatr Gerontol Int. 2017;17(2):295–301. https://doi.org/10.1111/ggi.12715.
Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia: changes over the years. Dysphagia. 2017;32(1):27–38. https://doi.org/10.1007/s00455-016-9775-x.
Farneti D, Fattori B, Bastiani L. The endoscopic evaluation of the oral phase of swallowing (Oral-FEES, O-FEES): a pilot study of the clinical use of a new procedure. Acta Otorhinolaryngol Ital. 2017;37(3):201–6. https://doi.org/10.14639/0392-100X-1126.
Wu CH, Hsiao TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope. 1997;107(3):396–401.
Acknowledgements
We would like to thank Ute Nastali for acquisition of data, and Gerhard Schön and Jürgen Höder for statistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical Approval
The study was conducted in compliance with the Helsinki Declaration.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nienstedt, J.C., Müller, F., Rösler, A. et al. Presbyphagia Diagnostics Using M-Mode Ultrasound: Changes in the Tongue Movement Pattern. Dysphagia 35, 696–701 (2020). https://doi.org/10.1007/s00455-019-10076-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10076-z