Abstract
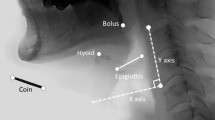
The purpose of this study was to conduct a quantitative analysis of the temporal and sequential events of the pharyngeal phase of swallowing in 45 poststroke patients who presented or did not present with supraglottic penetration and/or laryngotracheal aspiration and to compare the groups with each other and to a group of 46 patients with normal swallowing. All individuals were assessed by videofluoroscopy and the temporal and sequential measures for the swallowing of 3 mL and 5 mL of thickened liquid, 3 mL of liquid, and 3 mL and 5 mL of pasty were obtained by analyzing the recorded exams on Virtual Dub software. The following events were measured: time of maximal displacement and sustaining of the hyoid and larynx, duration of velopharyngeal sphincter (VS) and supraglottic closure, total inversion time of the epiglottis, duration of pharyngeal constriction, and duration of upper esophageal sphincter (UES) opening. For the analysis of the temporal sequence, the initial time of larynx and hyoid elevation, VS closure, epiglottic inversion, supraglottic closure, pharyngeal constriction, and opening of the UES were obtained. For 5 mL of thickened liquid, the maximum hyoid elevation time was greater for patients with normal swallowing and the time the supraglottis remained closed was higher in the aspirators group. The time of pharyngeal constriction during swallowing of 3 mL of thickened liquid was lower in the aspirators group. During the swallowing of 3 mL of thin liquid, it was observed that in the aspirators group, the larynx took longer to reach its maximum elevation and the epiglottis took longer to complete its total inversion. The analysis of the temporal sequence showed that patients in the aspirators group presented greater disorganization with significant alteration of the time interval between the events.





Similar content being viewed by others
References
Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia. 2001;16(1):7–18.
Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383–91.
Curtis DJ, Cruess DF, Dachman AH, Maso E. Timing in the normal pharyngeal swallow. Prospective selection and evaluation of 16 normal asymptomatic patients. Invest Radiol. 1984;19(6):523–9.
Inamoto Y, Fujii N, Saitoh E, Baba M, Okada S, Katada K, Ozeki Y, Kanamori D, Palmer JB. Evaluation of swallowing using 320-detector-row multislice CT. Part II: kinematic analysis of laryngeal closure during normal swallowing. Dysphagia. 2011;26(3):209–17.
Kang BS, Oh BM, Kim IS, Chung SG, Kim SJ, Han TR. Influence of aging on movement of the hyoid bone and epiglottis during normal swallowing: a motion analysis. Gerontology. 2010;56(5):474–82.
Kendall KA, Leonard RJ. Hyoid movement during swallowing in older patients with dysphagia. Arch Otolaryngol Head Neck Surg. 2001;127(10):1224–9.
Kendall KA, Leonard RJ. Pharyngeal constriction in elderly dysphagic patients compared with young and elderly nondysphagic controls. Dysphagia. 2001;16(4):272–8.
Kendall KA, McKenzie S, Leonard RJ, Gonçalves MI, Walker A. Timing of events in normal swallowing: a videofluoroscopic study. Dysphagia. 2000;15(2):74–83.
Kim Y, McCullough GH, Asp CW. Temporal measurements of pharyngeal swallowing in normal populations. Dysphagia. 2005;20(4):290–6.
Kim Y, McCullough GH. Maximal hyoid excursion in poststroke patients. Dysphagia. 2010;25(1):20–5. https://doi.org/10.1007/s00455-009-9224-1.
Kim Y, McCullough GH. Stage transition duration in patients poststroke. Dysphagia. 2007;22(4):299–305.
Lazarus CL, Logemann JA, Rademaker AW, Kahrilas PJ, Pajak T, Lazar R, Halper A. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993;74(10):1066–70.
Leonard R, Kendall KA, McKenzie S. Structural displacements affecting pharyngeal constriction in nondysphagic elderly and nonelderly adults. Dysphagia. 2004;19(2):133–41.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000;43(5):1264–74.
McConnel FM, Cerenko D, Jackson RT, Guffin TN Jr. Timing of major events of pharyngeal swallowing. Arch Otolaryngol Head Neck Surg. 1988;114(12):1413–8.
Molfenter SM, Steele CM. Kinematic and temporal factors associated with penetration-aspiration in swallowing liquids. Dysphagia. 2014;29(2):269–76.
Molfenter SM, Steele CM. Variation in temporal measures of swallowing: sex and volume effects. Dysphagia. 2013;28(2):226–33.
Nam HS, Oh BM, Han TR. Temporal characteristics of hyolaryngeal structural movements in normal swallowing. Laryngoscope. 2015;125(9):2129–33.
Ohmae Y, Logemann JA, Kaiser P, Hanson DG, Kahrilas PJ. Timing of glottic closure during normal swallow. Head Neck. 1995;17(5):394–402.
Rademaker AW, Pauloski BR, Logemann JA, Shanahan TK. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J Speech Hear Res. 1994;37(2):314–25.
Olthoff A, Zhang S, Schweizer R, Frahm J. On the physiology of normal swallowing as revealed by magnetic resonance imaging in real time. Gastroenterol Res Pract. 2014;2014:493174.
Hiss SG, Strauss M, Treole K, Stuart A, Boutilier S. Swallowing apnea as a function of airway closure. Dysphagia. 2003;18:293–300.
Vandaele DJ, McCulloch TM, Palmer PM, Langmore SE. Timing of glottic closure during swallowing: a combined electromyographic and endoscopic analysis. Ann Otol Rhinol Laryngol. 2005;114(6):478–87.
Power ML, Hamdy S, Singh S, Tyrrell PJ, Turnbull I, Thompson DG. Deglutitive laryngeal closure in stroke patients. J Neurol Neurosurg Psychiatry. 2007;78(2):141–6.
Choi KH, Ryu JS, Kim MY, Kang JY, Yoo SD. Kinematic analysis of dysphagia: significant parameters of aspiration related to bolus viscosity. Dysphagia. 2011;26(4):392–8.
Park T, Kim Y, Ko DH, McCullough G. Initiation and duration of laryngeal closure during the pharyngeal swallow in post-stroke patients. Dysphagia. 2010;25(3):177–82.
Power ML, Hamdy S, Goulermas JY, Tyrrell PJ, Turnbull I, Thompson DG. Predicting aspiration after hemispheric stroke from timing measures of oropharyngeal bolus flow and laryngeal closure. Dysphagia. 2009;24(3):257–64.
Seo HG, Oh BM, Han TR. Longitudinal changes of the swallowing process in subacute stroke patients with aspiration. Dysphagia. 2011;26(1):41–8.
Gay T, Rendell JK, Spiro J. Oral and laryngeal muscle coordination during swallowing. Laryngoscope. 1994;104(3 Pt 1):341–9.
Shaker R, Dodds WJ, Dantas RO, Hogan WJ, Arndorfer RC. Coordination of deglutitive glottic closure with oropharyngeal swallowing. Gastroenterology. 1990;98(6):1478–84.
Zamir Z, Ren J, Hogan WJ, Shaker R. Coordination of deglutitive vocal cord closure and oral-pharyngeal swallowing events in the elderly. Eur J Gastroenterol Hepatol. 1996;8(5):425–9.
Kendall KA, Leonard RJ, McKenzie SW. Sequence variability during hypopharyngeal bolus transit. Dysphagia. 2003;18(2):85–91.
Martin-Harris B, Brodsky MB, Price CC, Michel Y, Walters B. Temporal coordination of pharyngeal and laryngeal dynamics with breathing during swallowing: single liquid swallows. J Appl Physiol. 2003;94(5):1735–43.
Cook IJ, Dodds WJ, Dantas RO, Massey B, Kern MK, Lang IM, Brasseur JG, Hogan WJ. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989;257:G748–G759759.
Jacob P, Kahrilas PJ, Logemann JA, Shah V, Ha T. Upper esophageal sphincteropening and modulation during swallowing. Gastroenterology. 1989;97(6):1469–78.
Ren J, Shaker R, Zamir Z, Dodds WJ, Hogan WJ, Hoffmann RG. Effect of age and bolus variables on the coordination of the glottis and upper esophageal sphincter during swallowing. Am J Gastroenterol. 1993;88(5):665–9.
Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia. 1989;4(2):90–4.
Mendell DA, Logemann JA. Temporal sequence of swallow events during the oropharyngeal swallow. J Speech Lang Hear Res. 2007;50(5):1256–71.
Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. J Speech Lang Hear Res. 2002;45(3):434–45.
Vandaele DJ, Perlman AL, Cassell MD. Intrinsic fibre architecture and attachments of the human epiglottis and their contributions to the mechanism of deglutition. J Anat. 1995;186(Pt 1):1–15.
Herzberg EG, Lazarus CL, Steele CM, Molfenter SM. Swallow event sequencing: comparing healthy older and younger adults. Dysphagia. 2018;33:759–67.
Butler SG, Stuart A, Castell D, Russell GB, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume on pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52(1):240–53.
Selley WG, Flack FC, Ellis RE, Brooks WA. Respiratory patterns associated with swallowing: part 2. Neurologically impaired dysphagic patients Age Ageing. 1989;18(3):173–6.
Nilsson H, Ekberg O, Bülow M, Hindfelt B. Assessment of respiration during video fluoroscopy of dysphagic patients. Acad Radiol. 1997;4(7):503–7.
Leslie P, Drinnan MJ, Ford GA, Wilson JA. Swallow respiration patterns in dysphagic patients following acute stroke. Dysphagia. 2002;17(3):202–7.
Yotsuya H, Saito Y, Ide Y. Studies on temporal correlations of the movements of the pharyngeal organs during deglutition by X-ray TV cinematography. Bull Tokyo Dent Coll. 1981;22(3):171–81.
Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL. Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Lang Hearing Res. 1994;37(5):1041–9.
Rofes L, Arreola V, Romea M, Palomera E, Almirall J, Cabré M, Serra-Prat M, Clavé P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil. 2010;22:851–8.
Clavé P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, Serra-Prat M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24(9):1385–94.
Shaker R, Kern M, Bardan E, Taylor A, Stewart ET, Hoffmann RG, et al. Augmentation of deglutitive upper esophageal sphincter opening in the elderly by exercise. Am J Physiol. 1997;272:G1518–G15221522.
Fujiu M, Logemann J. Effect of a tongue-holding maneuver on posterior pharyngeal wall movement during deglutition. Am J Speech Lang Pathol. 1996;5:23–30.
Bulow M, Olsson R, Ekberg O. Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in patients with pharyngeal dysfunction. Dysphagia. 2001;16(3):190–5.
Acknowledgements
This study was performed in Department of Speech-Language Pathology and Audiology, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saconato, M., Leite, F.C., Lederman, H.M. et al. Temporal and Sequential Analysis of the Pharyngeal Phase of Swallowing in Poststroke Patients. Dysphagia 35, 598–615 (2020). https://doi.org/10.1007/s00455-019-10069-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10069-y