Abstract
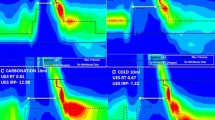
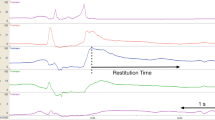
The purposes of this human study using high-resolution manometry were to verify whether the swallowing reflex can be evoked by intra-esophageal fluid injection and whether the reflex latency and manometric variables differ depending on the injected location, amount, or speed. Ten healthy individuals participated in this study. The tip of the intranasal catheter for injection was placed at 5 cm (upper), 10 cm (upper-middle), 15 cm (lower-middle), or 20 cm (lower) from the distal end of the upper esophageal sphincter (UES). An intra-esophageal injection of 3 mL or 10 mL of thickened water was administered and controlled at 3 mL/s or 10 mL/s. Latencies from the start of the injection to the onset of UES relaxation were compared regarding injection locations, amounts, and rates. Manometric variables of intra-esophageal injection and voluntary swallowing were compared. The latency became shorter when the upper region was injected. Latency after the 10-mL injection was shorter than that after the 3-mL injection (p < 0.01) when faster injection (10 mL/s) was used. Faster injection induced shorter latency (p < 0.01) when a larger volume (10 mL) was injected. Pre-maximum and post-maximum UES pressures during voluntary swallowing or during spontaneous swallowing when injecting the upper esophageal region were significantly higher than spontaneous swallowing at other regions (p < 0.01). Intra-esophageal fluid injection induces the swallowing reflex in humans. The most effective condition for inducing the swallowing reflex involved a larger fluid amount with a faster injection rate in the upper esophagus.








Similar content being viewed by others
References
Enzmann DR, Harell GS, Zboralske FF. Upper esophageal responses to intraluminal distention in man. Gastroenterology. 1977;72:1292–8.
Torrico S, Kern M, Aslam M, Narayanan S, Kannappan A, Ren J, Sui Z, Hofmann C, Shaker R. Upper esophageal sphincter function during gastroesophageal reflux events revisited. Am J Physiol Gastrointest Liver Physiol. 2000;279:G262–267.
Gerhardt DC, Shuck TJ, Bordeaux RA, Winship DH (1978) Human upper esophageal sphincter. Response to volume, osmotic, and acid stimuli. Gastroenterology 75(2), 268–274.
Aslam M, Kern M, Shaker R. Modulation of oesophago-UOS contractile reflex: effect of proximal and distal esophageal distention and swallowing. Neurogastroenterol Motil. 2003;15:323–9.
Babaei A, Dua K, Naini SR, Lee J, Katib O, Yan K, Hoffmann R, Shaker R. Response of the upper esophageal sphincter to esophageal distension is affected by posture, velocity, volume, and composition of the infusate. Gastroenterology. 2012;142(4):734–43.
Lang IM, Medda BK, Jadcherla SR, Shaker R. Characterization and mechanisms of the pharyngeal swallow activated by stimulation of the esophagus. Am J Physiol Gastrointest Liver Physiol. 2016;311(5):G827–G837837.
Taniguchi H, Aoyagi Y, Matsuo K, Nakagawa K, Saitoh E. Development of an esophageal stimulation method to elicit swallowing reflex in humans. J Oral Rehabil. 2017;45(3):211–5.
Hoffman MR, Ciucci MR, Mielens JD, Jiang JJ, McCulloch TM. Pharyngeal swallow adaptations to bolus volume measured with high-resolution manometry. Laryngoscope. 2010;120:2367–73.
Lin T, Xu G, Dou Z, Lan Y, Yu F, Jiang L. Effect of bolus volume on pharyngeal swallowing assessed by high-resolution manometry. Physiol Behav. 2014;128:46–51.
Matsubara K, Kumai Y, Samejima Y, Yumoto E. Swallowing pressure and pressure profiles in young healthy adults. Laryngoscope. 2014;124:711–7.
Hashmi S, Rao SS, Summers RW, Schulze K. Esophageal pressure topography, body position, and hiatal hernia. J Clin Gastroenterol. 2014;48:224–30.
Hasan Y, Go J, Hashmi SM, Valestin J, Schey R. Influence of everyday bolus consistencies in different body positions on high-resolution esophageal pressure topography (HREPT) parameters. Dis Esophagus. 2015;28:246–52.
Babaei A, Bhargava V, Mittal RK. Upper esophageal sphincter during transient lower esophageal sphincter relaxation: effects of reflux content and posture. Am J Physiol Gastrointest Liver Physiol. 2010;298:G601–607.
Zhang XJ, Xiang XL, Tu L, Xie XP, Hou XH. The effect of position on esophageal structure and function determined with solid-state high-resolution manometry. J Dig Dis. 2015;16:350–6.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–655.
McCulloch TM, Hoffman MR, Ciucci MR. High-resolution manometry of pharyngeal swallow pressure events associated with head turn and chin tuck. Ann Otol Rhinol Laryngol. 2010;119:369–76.
Hoffman MR, Mielens JD, Ciucci MR, Jones CA, Jiang JJ, McCulloch TM. High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn maneuver. Dysphagia. 2012;27:418–26.
Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–885.
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1033–1040.
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G988–997.
Paterson WG. Esophageal peristalsis. GI Motil Online. 2006. https://doi.org/10.1038/gimo13.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE. The Chicago Classification of esophageal motility disorders. Neurogastroenterol Motil. 2015;27:160–74.
Yahagi R, Okuda-Akabane K, Fukami H, Matsumoto N, Kitada Y. Facilitation of voluntary swallowing by chemical stimulation of the posterior tongue and pharyngeal region in humans. Neurosci Lett. 2008;448:139–42.
Kijima M, Isono S, Nishino T. Coordination of swallowing and phases of respiration during added respiratory loads in awake subjects. Am J Respir Crit Care Med. 1999;159:1898–902.
Jung KW, Jung HY, Myung SJ, Kim SO, Lee J, Yoon IJ, Seo SY, Lee JH, Kim DH, Choi KD, Song HJ, Lee GH, Murray JA, Romero Y, Kim JH. The effect of age on the key parameters in the Chicago classification: a study using high-resolution esophageal manometry in asymptomatic normal individuals. Neurogastroenterol Motil. 2015;27:246–57.
Creamer B, Schlegel J. Motor responses of the esophagus to distention. J Appl Physiol. 1957;10:498–504.
Woodland P, Aktar R, Mthunzi E, Lee C, Peiris M, Preston SL, Blackshaw LA, Sifrim D. Distinct afferent innervation patterns within the human proximal and distal esophageal mucosa. Am J Physiol Gastrointest Liver Physiol. 2015;308:G525–531.
Tsujimura T, Udemgba C, Inoue M, Canning BJ. Laryngeal and tracheal afferent nerve stimulation evokes swallowing in anaesthetized guinea pigs. J Physiol. 2013;591:4667–799.
Szczesniak MM, Fuentealba SE, Burnett A, Cook IJ. Differential relaxation and contractile responses of the human upper esophageal sphincter mediated by interplay of mucosal and deep mechanoreceptor activation. Am J Physiol Gastrointest Liver Physiol. 2008;294:G982–988.
Sengupta JN, Kauvar D, Goyal RK. Characteristics of vagal esophageal tension-sensitive afferent fibers in the opossum. J Neurophysiol. 1989;61:1001–100.
Lang IM, Medda BK, Shaker R. Mechanisms of reflexes induced by esophageal distension. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1246–1263.
Lang IM, Shaker R. Anatomy and physiology of the upper esophageal sphincter. Am J Med. 1997;103:50S–5S.
Lang IM, Medda BK, Jadcherla S, Shaker R. The role of the superior laryngeal nerve in esophageal reflexes. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1445–1457.
Steele CM, Miller AJ. Sensory input pathways and mechanisms in swallowing: a review. Dysphagia. 2010;25:323–33.
Lang IM. The physiology of eructation. Dysphagia. 2016;31:121–33.
Hwang K. Mechanism of transportation of the content of the esophagus. J Appl Physiol. 1954;6:781–96.
He M, Ohrui T, Azumi M, Ida S, Sasaki H. Depressed involuntary swallowing and risk of pneumonia. J Am Geriatr Soc. 2004;52:1032–3.
Acknowledgements
The authors thank Drs. Takanori Tsujimura and Makoto Inoue of the Division of Dysphagia Rehabilitation at Niigata University Graduate School of Medical and Dental Sciences for their valuable advice regarding this research.
Funding
This research was supported by a research grant-in-aid for Scientific Research C (no. 25862078 and 16K01477) from the Japanese Ministry of Education, Science, Culture, Sports, Science, and Technology.
Author information
Authors and Affiliations
Contributions
Hiroshige Taniguchi, Yoichiro Aoyagi, Sayuri Imaeda, and Makoto Hirumuta made substantial contributions to the conception, design, acquisition, analysis, and interpretation of data. Hiroshige Taniguchi and Yoichiro Aoyagi participated in drafting the paper or revising it critically for important intellectual content. Yoichiro Aoyagi, Koichiro Matsuo, and Eiichi Saitoh provided final approval of the version to be submitted and any revised version.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Taniguchi, H., Aoyagi, Y., Matsuo, K. et al. Elicitation of the Swallowing Reflex by Esophageal Stimulation in Healthy Subjects: An Evaluation Using High-Resolution Manometry. Dysphagia 35, 657–666 (2020). https://doi.org/10.1007/s00455-019-10068-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10068-z