Abstract
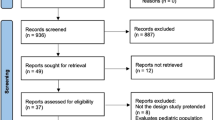
Most Zenker’s diverticula (ZD) cohort studies are single-institution retrospective observational studies of recurrence rates. There is a gap in the literature regarding patient-reported outcomes after ZD surgery. This study was conducted to compare if open transcervical diverticulectomy (OD) is better than endoscopic laser diverticulectomy (ELD) or endoscopic stapler-assisted diverticulectomy (ESD). The study design is of systematic review and meta-analysis. The following databases were searched: SCOPUS, EMBASE, PubMed, and Word of Science through December 2017. The quality of the studies was evaluated using 22-item STROBE checklist with 3 independent physician reviewers. The Inter-rater reliability was calculated both as a percent and utilizing Cohen’s Kappa. For the meta-analysis, Cohen’s d for an effect size was calculated for all studies comparing dysphagia results before and after surgery. A total of 865 patients were treated across 11 selected publications, of which 106 patients were treated OD, 310 ELD, and 449 with an ESD approach. Patient-reported dysphagia outcomes were reported as Cohen’s d (confidence interval): OD, ELD, and ESD were 1.31 (0.88, 1.74), 1.91 (1.62, 2.20), and 2.45 (2.04, 2.86), respectively. The pooled effect of all studies for dysphagia was 2.22 (1.85, 2.59) and regurgitation 2.20 (1.80, 2.59). We did not prove that OD has superior outcomes compared to ESD and ELD. Any method of surgical intervention yields a large effect (i.e., improvement in dysphagia and regurgitation) comparing patient-reported symptoms before and after surgery. Future research, currently underway, includes a prospective, multi-institutional study comparing standardized outcomes between treatments of ZD including symptom resolution, complications, and recurrences using validated measures to define long-term outcomes.
Level of Evidence 3



Similar content being viewed by others
References
Mosher H. Webs and pouches of the oesophagus, thier diagnosis and treatment. Surg Gynecol Obstet. 1917;25:175–87.
Bock JM, Van Daele DJ, Gupta N, Blumin JH. Management of Zenker’s diverticulum in the endoscopic age: Current practice patterns. Ann Otol Rhinol Laryngol. 2011;120(12):796–806.
Wilken R, Whited C, Scher RL. Endoscopic staple diverticulostomy for zenker’s diverticulum: review of experience in 337 cases. Ann Otol Rhinol Laryngol. 2015;124(1):21–9.
Parker NP, Misono S. Carbon dioxide laser versus stapler-assisted endoscopic zenker’s diverticulotomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2014;150(5):750–3.
Verdonck J, Morton RP. Systematic review on treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2015;272(11):3095–107.
Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–24.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Adam SI, Paskhover B, Sasaki CT. Laser versus stapler: Outcomes in endoscopic repair of Zenker diverticulum. Laryngoscope. 2012;122(9):1961–6.
Adam SI, Paskhover B, Sasaki CT. Revision zenker diverticulum: laser versus stapler outcomes following initial endoscopic failure. Ann Otol Rhinol Laryngol. 2013;122(4):247–53.
Bonavina L, Aiolfi A, Scolari F, Bona D, Lovece A, Asti E. Long-term outcome and quality of life after transoral stapling for zenker diverticulum. World J Gastroenterol. 2015;21(4):1167–72.
Colombo-Benkmann M, Unruh V, Krieglstein C, Senninger N. Cricopharyngeal myotomy in the treatment of zenker’s diverticulum. J Am Coll Surg. 2003;196(3):370–7 discussion 377; author reply 378.
Lang RA, Spelsberg FW, Winter H, Jauch KW, Huttl TP. Transoral diverticulostomy with a modified endo-gia stapler: Results after 4 years of experience. Surg Endosc. 2007;21(4):532–6.
Leibowitz JM, Fundakowski CE, Abouyared M, et al. Surgical techniques for Zenker’s diverticulum: a comparative analysis. Otolaryngol Head Neck Surg. 2014;151(1):52–8.
Miller FR, Bartley J, Otto RA. The endoscopic management of zenker diverticulum: CO2 laser versus endoscopic stapling. Laryngoscope. 2006;116(9):1608–11.
Murer K, Soyka MB, Broglie MA, Huber GF, Stoeckli SJ. Zenker’s diverticulum: outcome of endoscopic surgery is dependent on the intraoperative exposure. Eur Arch Otorhinolaryngol. 2015;272(1):167–73.
Peracchia A, Bonavina L, Narne S, Segalin A, Antoniazzi L, Marotta G. Minimally invasive surgery for Zenker diverticulum: analysis of results in 95 consecutive patients. Arch Surg. 1998;133(7):695–700.
Rodella L, Saladino E, Lombardo F, et al. Endoscopic diverticulostomy for Zenker’s diverticulum experience on 123 cases. G Chir. 2010;31(4):180–5.
Stoeckli SJ, Schmid S. Endoscopic stapler-assisted diverticuloesophagostomy for zenker’s diverticulum: patient satisfaction and subjective relief of symptoms. Surgery. 2002;131(2):158–62.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–35.
Lipsey MWWD, editor. Practical meta-analysis. 1st ed. Thousand Oaks, CA: Sage Pulications; 2000.
Ludlow A. A case of obstructed deglutition from a preternatural dilation of and bag formed in the pharynx. Med Observ Inquiries. 1769;3:85–101.
Zenker F, von Ziemssen H. Dilatations of the esophagus. Cycl Pr Med. 1878;3:46–8.
Hendriksma M, Joosten MH, Peters JP, Grolman W, Stegeman I. Evaluation of the quality of reporting of observational studies in otorhinolaryngology—based on the STROBE statement. PLoS ONE. 2017;12(1):e0169316.
Colpaert C, Vanderveken OM, Wouters K, Van de Heyning P, Van Laer C. Changes in swallowing-related quality of life after endoscopic treatment for zenker’s diverticulum using SWAL-QOL questionnaire. Dysphagia. 2017;32(3):339–44.
Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919–24.
Johnson CM, Postma GN. Zenker diverticulum—which surgical approach is superior? JAMA Otolaryngol Head Neck Surg. 2016;142(4):401–3.
Venkatesan NN, Evangelista LM, Kuhn MA, Belafsky PC. Normal fluoroscopic appearance status post-successful endoscopic zenker diverticulotomy. Laryngoscope. 2017;127(8):1762–6.
Leonard R, Rees CJ, Belafsky P, Allen J. Fluoroscopic surrogate for pharyngeal strength: the pharyngeal constriction ratio (PCR). Dysphagia. 2011;26(1):13–7.
Berzofsky CE, Holiday RA, Pitman MJ. Variability of postoperative esophagrams after endoscopic cricopharyngeal myotomy: technique dependence. Ann Otol Rhinol Laryngol. 2012;121(3):145–50.
Bonavina L, Bona D, Abraham M, Saino G, Abate E. Long-term results of endosurgical and open surgical approach for zenker diverticulum. World J Gastroenterol. 2007;13(18):2586–9.
Rosen SP, Jones CA, McCulloch TM. Pharyngeal swallowing pressures in the base-of-tongue and hypopharynx regions identified with three-dimensional manometry. Laryngoscope. 2017;127(9):1989–95.
Acknowledgements
We would like to thank our librarian Mr. Don Jason for his expertise during our literature search. We would also like to thank Dr. Luigi Bonavina for providing additional details to meet our inclusion criteria.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Howell, R.J., Giliberto, J.P., Harmon, J. et al. Open Versus Endoscopic Surgery of Zenker’s Diverticula: A Systematic Review and Meta-analysis. Dysphagia 34, 930–938 (2019). https://doi.org/10.1007/s00455-019-09994-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-09994-9