Abstract
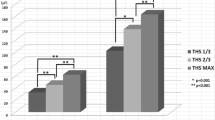
This study investigated differences in suprahyoid muscle activity in elderly adults during tongue-hold swallowing (THS) according to tongue protrusion length to determine the most effective tongue protrusion length during THS. A total of 52 healthy participants (34 females and 18 males) aged 69–92 years were included. Changes in suprahyoid muscle activation during normal swallowing and THS with 1/3rd and 2/3rd tongue protrusions using surface electromyography were observed. Suprahyoid muscle activation significantly increased with the increasing tongue protrusion length (p < 0.05). Depending on the responses of the participants based on tongue protrusion length, participants were categorized into the increase group [increased suprahyoid muscle activity with tongue protrusion, n = 36 (1/3rd THS compared to normal swallowing) or 38 (2/3rd THS compared to normal swallowing)] or decrease group [decreased suprahyoid muscle activity with tongue protrusion, n = 16 (1/3rd THS compared to normal swallowing) or 14 (2/3rd THS compared to normal swallowing)]. The functional reserve of the increase group was significantly higher than that of the decrease group (p < 0.05). Many elderly people were found to have increased activation of the suprahyoid muscle during THS; however, others showed the opposite. Therefore, it is necessary to confirm the degree of suprahyoid muscle activation during THS so that the patient can perform the exercise at the tongue protrusion length that can maximize the effect of the exercise. For individuals who cannot overcome even a small amount of tongue protrusion (e.g., 1/3rd MTPL), replacing THS with another exercise may be considered.



Similar content being viewed by others
References
Fujiu M, Logemann JA, Pauloski BR. Increased postoperative posterior pharyngeal wall movement in patients with anterior oral cancer: preliminary findings and possible implications for treatment. Am J Speech Lang Pathol. 1995;4:24–30.
Kahrilas PJ, Logemann JA, Lin S, Ergun GA. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992;103:128–36.
McConnel FM. Analysis of pressure generation and bolus transit during pharyngeal swallowing. Laryngoscope. 1988;98:71–8.
Fujiu MA, Logemann J. Effect of a tongue-holding maneuver on posterior pharyngeal wall movement during deglutition. Am J Speech Lang Pathol. 1996;5:23–30.
Burkhead LM, Sapienza CM, Rosenbek JC. Strength-training exercise in dysphagia rehabilitation: principles, procedures, and directions for future research. Dysphagia. 2007;22:251–65.
Doeltgen SH, Witte U, Gumbley F, Huckabee ML. Evaluation of manometric measures during tongue-hold swallows. Am J Speech Lang Pathol. 2009;18:65–73.
Oh JC, Park JW, Cha TH, Woo HS, Kim DK. Exercise using tongue-holding swallow does not improve swallowing function in normal subjects. J Oral Rehabil. 2012;39:364–9.
Woo HS, Chang KY, Oh JC. The effects of eight week tongue-holding maneuver program on activation of swallowing related muscles. J Korean Soc Occup Ther. 2014;22:53–64.
Fujiu-Kurachi M, Fujiwara S, Tamine KI, Kondo J, Minagi Y, Maeda Y, Hori K, Ono T. Tongue pressure generation during tongue-hold swallows in young healthy adults measured with different tongue positions. Dysphagia. 2014;29:17–24.
Hammer MJ, Jones CA, Mielens JD, Kim CH, McCulloch TM. Evaluating the tongue-hold maneuver using high-resolution manometry and electromyography. Dysphagia. 2014;29:564–70.
Oh JC. Effects of tongue-hold swallows on suprahyoid muscle activation according to the relative tongue protrusion length: a preliminary study. Springerplus. 2016;5:1144.
Fujiwara S, Fujiu-Kurachi M, Hori K, Maeda Y, Ono T. Tongue pressure production and submental surface electromyogram activities during tongue-hold swallow with different holding positions and tongue length. Dysphagia. 2017;33(4):1–11.
Trapl M, Enderle P, Nowotny M, Teuschl Y, Matz K, Dachenhausen A, Brainin M. Dysphagia bedside screening for acute-stroke patients: the gugging swallowing screen. Stroke. 2007;38:2948–52.
Beckmann Y, Gürgör N, Çakır A, Arıcı Ş, İncesu TK, Seçil Y, et al. Electrophysiological evaluation of dysphagia in the mild or moderate patients with multiple sclerosis: a concept of subclinical dysphagia. Dysphagia. 2015;30:296–303.
Robbins JA, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88:150–8.
Robin DA, Goel A, Somodi LB, Luschei ES. Tongue strength and endurance: relation to highly skilled movements. J Speech Hear Res. 1992;35:1239–45.
Adams V, Mathisen B, Baines S, Lazarus C, Callister R. Reliability of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument with elderly adults. Disabil Rehabil. 2015;37:389–95.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707.
Sakamoto Y. Gross anatomical observations of attachments of the middle pharyngeal constrictor. Clin Anat. 2014;27:603–9.
Crary MA, Carnaby GD, Groher ME. Biomechanical correlates of surface electromyography signals obtained during swallowing by healthy adults. J Speech Lang Hear Res. 2006;49:186.
Perlman AL, Palmer PM, McCulloch TM, Vandaele DJ. Electromyographic activity from human laryngeal, pharyngeal, and submental muscles during swallowing. J Appl Physiol. 1999;86:1663–9.
Steele CM. Optimal approaches for measuring tongue-pressure functional reserve. J Aging Res. 2013;2013:542909.
Yeates EM, Steele CM, Pelletier CA. Tongue pressure and submental surface electromyography measures during noneffortful and effortful saliva swallows in healthy women. Am J Speech Lang Pathol. 2010;19:274–81.
Umeki H, Takasaki K, Enatsu K, Tanaka F, Kumagami H, Takahashi H. Effects of a tongue-holding maneuver during swallowing evaluated by high-resolution manometry. Otolaryngol Head Neck Surg. 2009;141:119–22.
Doeltgen SH, Macrae P, Huckabee ML. Pharyngeal pressure generation during tongue hold swallows across age groups. Am J Speech Lang Pathol. 2011;20:124–31.
Mishra A, Rajappa A, Tipton E, Malandraki GA. The recline exercise: comparisons with the head lift exercise in healthy adults. Dysphagia. 2015;30:730–7.
Slovarp L, King L, Off C, Liss J. A pilot study of the tongue pull-back exercise for improving tongue-base retraction and two novel methods to aadd resistance to the tongue pull-back. Dysphagia. 2016;31:416–23.
Acknowledgements
This work was supported by the research Grant of Cheongju University (2018.03.01–2020.02.29).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All the participants provided informed consents to participate in this study.
Rights and permissions
About this article
Cite this article
Oh, JC. Effects of Tongue-Hold Swallows on Suprahyoid Muscle Activation According to the Relative Tongue Protrusion Length in the Elderly Individuals. Dysphagia 34, 382–390 (2019). https://doi.org/10.1007/s00455-018-9948-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9948-x