Abstract
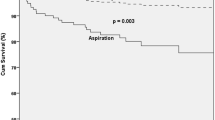
Nasogastric tube (NGT) is a common feeding strategy for patients at risk of endotracheal aspiration with an oral diet. With NGT feeding, however, swallowing of small amounts saliva cannot be avoided. We investigated whether the aspiration rate when swallowing 1 mL of fluid increased in patients using an NGT in different dysphagia severities. One hundred forty-seven patients who had been receiving NGT feeding underwent a videofluoroscopic swallowing study (VFSS). During VFSS, subjects were offered 1 mL of fluid twice: initially, with the tube inserted (NGT-in) and, subsequently, with the tube removed (NGT-out). Aspiration depth was determined using the 8-point Penetration–Aspiration Scale (PAS) (0 points, no aspiration/penetration; 8 points, aspiration passing the vocal cords with no ejection efforts). PAS-diff was computed (PASNGT-in − PASNGT-out), and a positive PAS-diff (PAS-diff > 0) meant increased aspiration depth in the presence of NGT. After VFSS, diet recommendations were made according to dysphagia severity assessment: non-oral feeding (n = 59), diet modification (n = 74), and diet as tolerated (n = 13). Cognitive level (mini-mental state examination, MMSE) and general functional level (Modified Barthel Index, MBI) were compared between the PAS-diff > 0 and PAS-diff ≤ 0 groups. Aspiration severity did not significantly change after NGT removal (PASNGT-in, 2.45 ± 2.40; PASNGT-out, 2.57 ± 2.58; P = .50). Regardless of recommended diet, PAS-diff values were not significantly different (P = .49). MMSE and MBI were not significantly different (P = .23 and .94) between subjects with PAS-diff > 0 (n = 25) and PAS-diff ≤ 0 (n = 121). In conclusion, the risk of aspirating a small amount of fluid was not significantly different before and after NGT removal, regardless of swallowing function, cognitive level, or general functional level.


Similar content being viewed by others
References
Vanek VW. Ins and outs of enteral access. Part 1: short-term enteral access. Nutr Clin Pract. 2002;17:275–83.
National Patient Safety Agency. Quarterly data summary issue 9: learning from reporting—nasogastric tube incidents. 2008 http://www.nrls.npsa.nhs.uk/resources/collections/quarterly-data-summaries.
Groher ME, Groher TP. When safe oral feeding is threatened: end-of-life options and decisions. Top Lang Disorders. 2012;32:149–67.
Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: final data for 2014. Natl Vital Stat Rep. 2016;65:1–122.
Finucane TE, Bynum JP. Use of tube feeding to prevent aspiration pneumonia. Lancet. 1996;348:1421–4.
Dziewas R, Ritter M, Schilling M, Konrad C, Oelenberg S, Nabavi DG, Stogbauer F, Ringelstein EB, Ludemann P. Pneumonia in acute stroke patients fed by nasogastric tube. J Neurol Neurosurg Psychiatry. 2004;75:852–6.
Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103:823–9.
Huggins PS, Tuomi SK, Young C. Effects of nasogastric tubes on the young, normal swallowing mechanism. Dysphagia. 1999;14:157–61.
Gates J, Hartnell GG, Gramigna GD. Videofluoroscopy and swallowing studies for neurologic disease: a primer. Radiographics. 2006;26:e22.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11:93–8.
Kwon YC, Park J-H. Korean version of mini-mental state examination (MMSE-K). Part I: development of the test for the elderly. J Korean Neuropsychiatr Assoc. 1989;28:125–35.
Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, Kim SH, Kim TH, Han TR. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehab Med. 2007;31:283–97.
Mamun K, Lim J. Role of nasogastric tube in preventing aspiration pneumonia in patients with dysphagia. Singapore Med J. 2005;46:627–31.
Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Ramirez-Perez C. Complications associated with enteral nutrition by nasogastric tube in an internal medicine unit. J Clin Nurs. 2001;10:482–90.
Gomes GF, Pisani JC, Macedo ED, Campos AC. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care. 2003;6:327–33.
Valles J, Artigas A, Rello J, Bonsoms N, Fontanals D, Blanch L, Fernandez R, Baigorri F, Mestre J. Continuous aspiration of subglottic secretions in preventing ventilator-associated pneumonia. Ann Intern Med. 1995;122:179–86.
Lagerlof F, Dawes C. The volume of saliva in the mouth before and after swallowing. J Dent Res. 1984;63:618–21.
Kim IS, Han TR. Influence of mastication and salivation on swallowing in stroke patients. Arch Phys Med Rehabil. 2005;86:1986–90.
Ibanez J, Penafiel A, Raurich JM, Marse P, Jorda R, Mata F. Gastroesophageal reflux in intubated patients receiving enteral nutrition: effect of supine and semirecumbent positions. JPEN J Parenter Enteral Nutr. 1992;16:419–22.
Satou Y, Oguro H, Murakami Y, Onoda K, Mitaki S, Hamada C, Mizuhara R, Yamaguchi S. Gastroesophageal reflux during enteral feeding in stroke patients: a 24-hour esophageal pH-monitoring study. J Stroke Cerebrovasc Dis. 2013;22:185–9.
Metheny NA, Clouse RE, Chang YH, Stewart BJ, Oliver DA, Kollef MH. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med. 2006;34:1007–15.
Wang TG, Wu MC, Chang YC, Hsiao TY, Lien IN. The effect of nasogastric tubes on swallowing function in persons with dysphagia following stroke. Arch Phys Med Rehabil. 2006;87:1270–3.
Fattal M, Suiter DM, Warner HL, Leder SB. Effect of presence/absence of a nasogastric tube in the same person on incidence of aspiration. Otolaryngol Head Neck Surg. 2011;145:796–800.
Leder SB, Suiter DM. Effect of nasogastric tubes on incidence of aspiration. Arch Phys Med Rehabil. 2008;89:648–51.
Oto T, Kandori Y, Ohta T, Domen K, Koyama T. Predicting the chance of weaning dysphagic stroke patients from enteral nutrition: a multivariate logistic modelling study. Eur J Phys Rehabil Med. 2009;45:355–62.
Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U. Predictors of survival after severe dysphagic stroke. J Neurol. 2005;252:1510–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
None of the authors has any proprietary interests in the materials described in this article. This study protocol was approved by our institutional review board.
Informed Consent
We retrospectively reviewed the medical records, and informed consent was waived.
Rights and permissions
About this article
Cite this article
Kim, G., Baek, S., Park, Hw. et al. Effect of Nasogastric Tube on Aspiration Risk: Results from 147 Patients with Dysphagia and Literature Review. Dysphagia 33, 731–738 (2018). https://doi.org/10.1007/s00455-018-9894-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9894-7